Table of Contents
Renin Angiotensin System (RAS) blockers are renoprotective and often used in chronic kidney disease (CKD). RAS blockers include:
- Angiotensin Converting Enzyme (ACE) Inhibitors
- Angiotensin Receptor Blockers (ARB)
These medications have proven benefits in proteinuric CKD Proteinuria: What is it and How I Treat | BCNephro , including microalbuminuria in patients with diabetic kidney disease.
- Non Diabetic CKD
- Greater benefit with greater proteinuria reduction
- No preferential benefit with proteinuria < 500 mg day as shown in AASK trial. Effect of Blood Pressure Lowering and Antihypertensive Drug Class on Progression of Hypertensive Kidney Disease: Results From the AASK Trial
- Diabetic CKD
- Delayed progression from microalbuminuria to macroalbuminuria as in this trial. The Effect of Irbesartan on the Development of Diabetic Nephropathy in Patients with Type 2 Diabetes | NEJM
- Decreased risk of death, dialysis and doubling of serum creatinine as in the IDNT trial. Renoprotective Effect of the Angiotensin-Receptor Antagonist Irbesartan in Patients with Nephropathy Due to Type 2 Diabetes | NEJM
Why does proteinuria occur and what does it mean? Here’s what I explain to patients.
- The kidneys filter the blood and the waste passes into the urine
- The kidneys contain about a million of these tiny kidney filters called glomeruli.
- The waste passes through these filters (glomeruli) and comes out in the urine, but protein is not supposed to fit through the filters and stays in the blood.
- If the glomeruli are damaged, protein can leak through and be excreted in the urine. This has 2 implications.
- It is a sign of a kidney disease that should be diagnosed and treated.
- The process of protein passing through the kidneys in the urine is nephrotoxic and is a risk factor for developing worsening kidney function (GFR). (Even if the kidney function (GFR) is normal this abnormality indicates kidney disease.)
- RAS blockers not only decrease the systemic blood pressure, they specifically decrease the pressure in the glomeruli therefore decreasing proteinuria and protecting the kidneys. This point is important for patients to know as they may stop the medication if their blood pressure is normal. The medication is still renoprotective even if the blood pressure is normal.
Normal Glomerular Physiology
Afferent arteriole goes into the glomerulus, Efferent arteriole leaves the glomerulus.
Glomerular pressure is maintained by dilation or constriction of the afferent and efferent arterioles.
- Afferent arteriole:
- Dilation – increased glomerular pressure – more pressure in
- Constriction – decreased glomerular pressure – less pressure in, the arteriolar pressure is blunted
- Efferent arteriole:
- Dilation – decreased glomerular pressure – less back pressure on glomerulus
- Constriction – increased glomerular pressure – more back pressure on glomerulus
How RAS blockers work:
- ACE inhibitors: decrease production of angiotensin
- ARB: block angiotensin binding to receptor
What does angiotensin do in the kidney?
- Angiotensin constricts the efferent arteriole, the arteriole that leaves the glomerulus.
- RAS blockers impair constriction of the efferent arteriole thereby decreasing glomerular pressure.
- Lower glomerular pressure leads to a decrease in proteinuria (less protein is pushed through the glomerulus)
How do RAS blockers affect the kidney?
- Decreased glomerular pressure leads to decreased proteinuria (less protein is pushed through glomeruli).
- Decreased proteinuria (and decreased blood pressures) leads to a slowing of CKD What? I have Stage 3 Kidney Disease!! Talking to patients about GFR and CKD | BCNephro
- However, there is a trade off. These medications may result in an increased serum creatinine. A creatinine increase of 30% over 6-8 weeks that stabilizes is considered to be acceptable and traditionally had been thought to be a marker of greater long term renoprotection. Angiotensin-Converting Enzyme Inhibitor–Associated Elevations in Serum Creatinine: Is This a Cause for Concern? | Cardiology | JAMA Internal Medicine
The way I describe it to patients is this. These medications make the kidneys work less hard, if they are working less hard they are less likely to burn out over time. I draw the following graph:
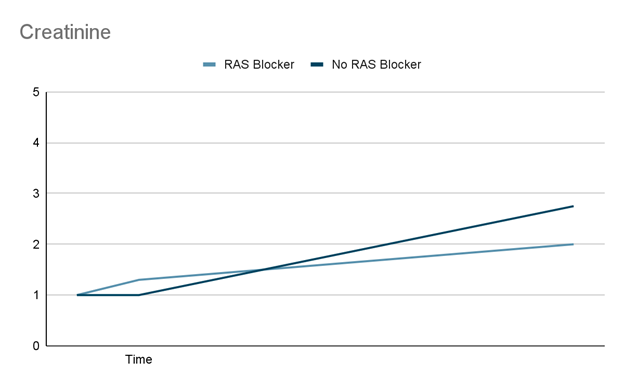
This graph is not an exact scientific projection of creatinine trend with and without RAS blockers, it is meant as an illustration that the initial acute increase in creatinine is expected to be associated with an overall slower progression of CKD and pay off in the long run.
Although an increase in creatinine with an RAS blocker of up to 30% is considered acceptable it is debatable that this is associated with improved outcomes.
This retrospective study Association of Acute Increases in Plasma Creatinine after Renin-Angiotensin Blockade with Subsequent Outcomes – PMC found that creatinine increases of > 10% after initiation of an RAS blocker was associated with an increased risk of:
- Mortality
- Cardiovascular events
- ESRD
However, this is a retrospective study and therefore the higher creatinine increases with RAS blockade may be a marker of more underlying disease severity. There is no evidence that discontinuing the medication in patients with a creatinine increase between 10 and 30% improves outcomes.
My Bottom Line: If the creatinine runs a little bit higher, but the proteinuria Proteinuria: What is it and How I Treat | BCNephro is significantly improved and the blood pressure is controlled, the patient is likely to be better off in the long run.
If there is a > 30% increase in serum creatinine with the initiation of an RAS blocker the medication should be discontinued. This may occur in:
- Bilateral renal artery stenosis
- Heart Failure
- CKD
In these cases if the RAS blocker resulted in a significant improvement in proteinuria and blood pressure and the creatinine increase is nominally > 30%, I may discontinue a different medication (such as a diuretic or SGLT 2 inhibitor) and repeat kidney function assessment in an attempt to allow continuation of the RAS blocker.
Potential Complications of RAS blockers
- There are certain situations where the kidneys need to constrict the efferent arteriole to maintain GFR. These include:
- Hypovolemia
- Hypotension
If the RAS blocker is continued in these situations, Acute Kidney Injury (AKI) from ischemic Acute Tubular Necrosis (ATN) can result. Therefore I counsel patients to hold the medication in these situations:
- A severe dehydrating illness such as gastroenteritis or food poisoning with severe diarrhea and an inability to take PO liquids.
- Preoperatively.
Combining RAS blockers (ACE inhibitors and ARBs) is associated with an increased risk of complications (hyperkalemia and acute kidney injury) as described in the ONTARGET trial https://www.nejm.org/doi/full/10.1056/nejmoa0801317 and should not be done.
My practice however is to cautiously combine RAS blockers with mineralocorticoid antagonists for improved proteinuria and BP control. This needs to be done cautiously with close monitoring of potassium and creatinine.
Other Complications of RAS blockers
- Hyperkalemia
- Rare if eGFR > 40 and potassium in the low – mid normal range.
- I repeat BMP 1-2 weeks after initiation or dose adjustment
- Counsel patients to avoid other meds that can increase potassium (NSAIDS, TMP – SMX).
- Concomitant use of diuretics (ie thiazides) may help control potassium.
- Cough
- Dry hacking cough with ACE-inhibitors
- Switch to ARB
- Angioedema
- Can occur with ACE inhibitors, rare with ARBs
- If angioedema occurs with an ACE inhibitor and was not severe (i.e. did not result in respiratory failure or require intubation) I offer an ARB. I counsel the patients that there is a low risk that angioedema may recur.
- Contraindicated during pregnancy
- Pancreatitis
- With ACE inhibitors
- Enteropathy
- With the ARB olmesartan
Should RAS blockers be stopped with advanced CKD?
There is a concern with advanced CKD that RAS blockers should be held. The concern is that when patients are approaching ESRD that holding these medications may help defer the need for RRT.
However there are studies that show these medications are still of benefit in stage 4 CKD. This trial Efficacy and Safety of Benazepril for Advanced Chronic Renal Insufficiency | NEJM showed that the ACE-I benazepril decreased the risk of death, doubling creatinine, or ESRD when used in stage 4 proteinuric CKD.
In addition there are trials that show that stopping RAS blockers in advanced progressive CKD is not beneficial in delaying progression to ESRD. The Stop ACEi trial Renin–Angiotensin System Inhibition in Advanced Chronic Kidney Disease | NEJM randomized patients with advanced progressive kidney disease to continue or stop RAS blocker.
- eGFR < 30 with a decrease of > 2 ml/min/yr for 2 years
- No difference at 3 years of
- eGFR: 12.6 (discontinuation group) vs 13.3 (continuation group)
- ESRD: 62% (discontinuation group) vs 56% (continuation group)
Despite this, I often hold RAS blockers in patients with progressive CKD that is approaching the need for RRT (eGFR < 15) https://bcnephro.com/counseling-patients-with-ckd-about-dialysis/ , in an attempt to “buy some time” before dialysis becomes necessary. My anecdotal observations are similar to what was found in the above studies.
- There are patients with advanced CKD that is stable who are able to continue the RAS blocker
- Many patients with progressive advanced progressive CKD have a continued worsening after discontinuation of the RAS blocker.
Summary
RAS blockers are a critical agent in the treatment of CKD. In using them be aware of the following considerations:
- The renal benefit is mainly in patients with proteinuria.
- Protein creatinine ratio > 500 mg/gram in non diabetic CKD
- Microalbuminuria (albumin creatinine ratio 30-300 mg/ gram or macroalbuminuria albumin creatinine ratio 30-300 mg/ gram) in diabetic CKD
- Monitor BMP closely after initiation or dose escalation.
- An increase in creatinine of <30% is acceptable, so long as it stabilizes
- Avoid combination ACE-I and ARBs
- Counsel patients to hold these medications with an acute severe dehydrating illness, perioperatively, or with acute use of other medication that raise potassium (NSAIDS; TMP-SMX)
- ARBs often can be safely used in patients with a history of angioedema on ACE inhibitors.
- Hyperkalemia can often be controlled with concomitant use of a thiazide diuretic.
- Be aware of other side effects, contraindication during pregnancy, cough with ACE inhibitors and enteropathy with olmesartan.



