Table of Contents
Bisphosphonates and denosumab are anti resorptive medications used for the treatment of:
- Osteoporosis
- Hypercalcemia, especially hypercalcemia of malignancy
Hypercalcemia, Nephrology and the Milk Alkali Syndrome @BCNephro
Hypercalcemia BCNephro
- Malignancy, particularly multiple myeloma and bone metastasis with solid tumors (prostate, breast, lung)
Both classes of medications exert their anti resorptive effects by inhibiting osteoclast activity.
- Bisphosphonates direct toxic effect on osteoclasts
- Denosumab impairs rank ligand (RANKL) which is important in osteoclast function.
Oral bisphosphonates, used for osteoporosis, have no significant nephrotoxicity and are not addressed in this article.
It is important to understand the potential adverse renal effects and use of these medications in chronic kidney disease as they are often used in conditions associated with abnormal kidney function, particularly hypercalcemia and multiple myeloma.
Bisphosphonates
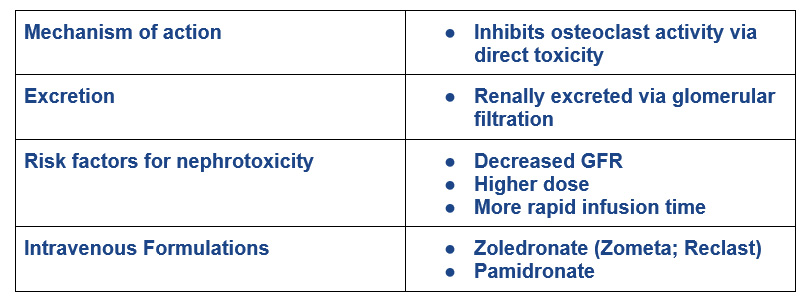
Nephrotoxicity is less common when intravenous formulations used for osteoporosis.
- Dosed less frequently
- One study showed AKI developed in 1.4% of elderly patients (age > 75) receiving zoledronic acid for osteoporosis. All these patients had a creatinine clearance > 45. Few patients in this study, only 4.5%, had a creatinine clearance < 35.
Renal safety of zoledronic acid for osteoporosis in adults 75 years and older
Zoledronic Acid
Zoledronic acid comes in two forms:
Reclast: Used for osteoporosis. Dosed 5 mg IV every 1-2 years
Zometa: Malignancy: Dosed 4 mg IV over 15 minutes every 4 weeks
Hypercalcemia: Dosed 4 mg IV over 15 minutes, may repeat after 7 days
Nephrotoxicity of zoledronic acid:
- Associated with acute kidney injury (AKI) on the basis of acute tubular necrosis (ATN)
- AKI more likely with shorter infusion times (5 vs 15 minutes) or higher dose (8 mg vs 4 mg)
- Most reports of AKI when used in treatment for multiple myeloma
- Case reports of Fanconi syndrome
- Typically not associated with glomerular disease/ proteinuria.
Check renal function prior to each dose.
Slowing infusion time to 30-60 minutes can be considered to decrease risk of nephrotoxicity.
Pamidronate
Typical dose is 90 mg over 2-4 hours.
Nephrotoxicity of pamidronate:
- Associated with the collapsing variant of focal segmental glomerulosclerosis (FSGS). Presenting as nephrotic proteinuria often with abnormal kidney function.
Focal Segmental Glomerulosclerosis @BCNephro
FSGS – Focal Segmental Glomerulosclerosis | BCNephro
- Reports of other glomerulopathies (non collapsing variant of FSGS and minimal change disease).
- AKI on the basis of ATN is a less common presentation.
With impaired kidney function I recommend:
- Ensure adequate intravenous hydration, particularly in patients presenting with severe hypercalcemia who often are hypovolemic and have AKI (hypercalcemia causes polyuria)
- Use a lower dose (i.e. 30 or 60 mg as opposed to 90 mg) over a longer infusion time (i.e. 6 hours)
Check renal function prior to each dose.
With chronic use, monitor urine protein every 3- 6 months,
Zoledronic acid vs Pamidronate
- Zoledronic acid preferred over pamidronate in multiple myeloma and solid tumors
- Shorter infusion time
- Greater potency
- Greater efficacy in solid tumors
- May have survival benefit in MM
- I consider zoledronic acid to be more nephrotoxic than pamidronate, as more likely to cause AKI via ATN
- Zoledronic acid is not recommended if eGFR is less than 30.
In patients with AKI or significant CKD, I prefer use of an attenuated dose of pamidronate with longer infusion times or the use of denosumab.
Denosumab
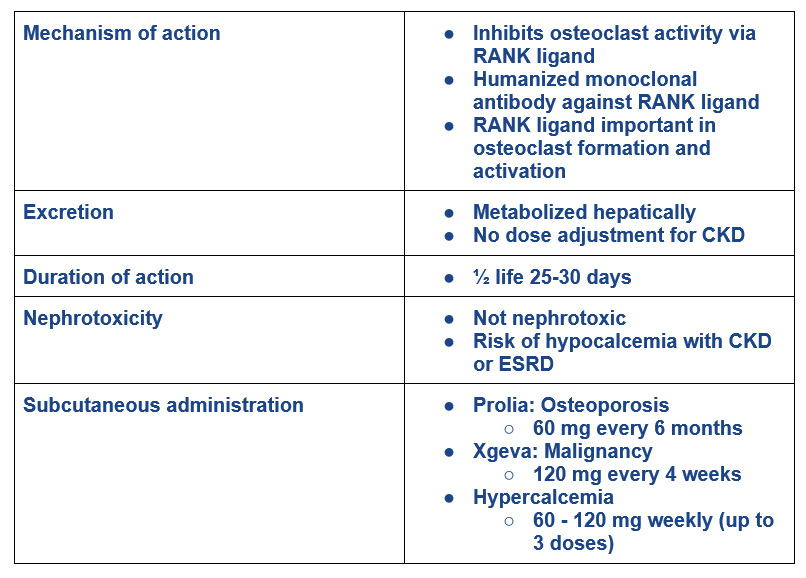
Hypocalcemia post denosumab:
- Risk factors include lower eGFR (<30), lower baseline calcium and higher alkaline phosphatase
- CKD – 10.4% asymptomatic hypocalcemia. ESRD 25-42%
- Nadir calcium 7-20 days, may persist for 2 months.
In patients with impaired kidney function
- Consider use of lower dose (60 mg)
- Correct vitamin D deficiency , hypocalcemia and hypomagnesemia prior to administration
- In patients with secondary hyperparathyroidism of renal origin, I would consider correcting with use of an active vitamin D such as calcitriol.
- Check calcium and PTH 2 weeks post infusion in CKD. Weekly (or more frequent) for 2 months in ESRD
Summary
Bisphosphonates and denosumab are medications that nephrologists should be familiar with. They are often used in conditions associated with acute kidney injury such as hypercalcemia and multiple myeloma. In addition intravenous bisphosphonates have potential nephrotoxicity and there is a significant risk of hypocalcemia when denosumab is used in chronic kidney disease,



