Table of Contents
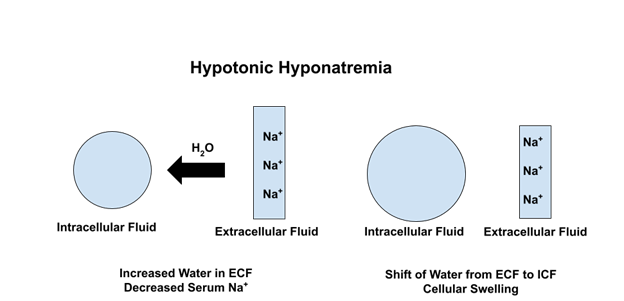
Hypotonic Hyponatremia
In most cases of hyponatremia there is an excess of H20 relative to Na in the body.
This decreases the tonicity (osmolality) of the serum. Water then moves from the extracellular to intracellular space down this osmotic gradient. This causes cellular swelling. Cellular swelling in the brain explains the adverse CNS effects of severe hyponatremia.
Translocational Hyponatremia
There is another mechanism of hyponatremia. That is an increase in the tonicity of serum from another osmotically active substance. In these situations the osmotic gradient works in reverse. Water moves from the intracellular to extracellular space. Therefore this is not associated with cellular swelling.
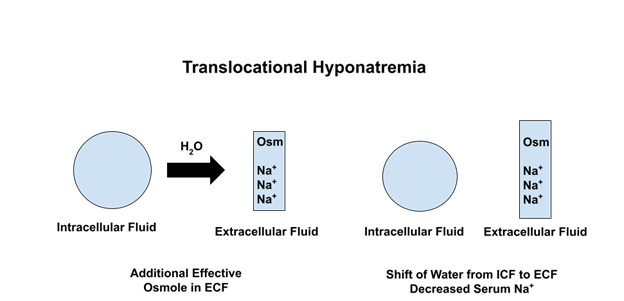
This is commonly seen in cases of severe hyperglycemia as in hyperglycemic hyperosmolar nonketotic syndrome (HHNK). When the hyperglycemia is treated water can move back from the extracellular to intracellular space and the hyponatremia corrects.
There are other causes of translocational hyponatremia, two of which I have encountered.
Case 1
A woman presented with severe acute kidney injury (AKI) and hyponatremia. She had been receiving a treatment course of intravenous immune globulin (IVIG) as an outpatient for a neurologic condition.
She required acute hemodialysis. Hyponatremia and AKI subsequently resolved.
IVIG has been associated with hyponatremia by several mechanisms. It can cause pseudohyponatremia as the protein can temporarily increase the solid component of plasma.
However, in this case I believe the major cause of hyponatremia was translocational.
IVIG requires a stabilizer which is typically a sugar. In the past sucrose was a common stabilizer in IVIG preparations.
In this case the AKI was caused by sucrose, which is known to be nephrotoxic. Because of the AKI the sucrose was retained (not renally excreted). The sucrose created an osmotic gradient for translocational hyponatremia.
As sucrose not uncommonly was associated with AKI it is not used as a stabilizer in current IVIG preparations. Other sugars, commonly maltose, are used. Although maltose is less nephrotoxic, nephrotoxicity can occur and it is osmotically active so hyponatremia may still be seen.
Case 2
A man with a history of cirrhosis and prostate cancer treated with radiation complicated by radiation cystitis. He was hospitalized with gross hematuria. Required cystoscopy with fulguration which was a complicated procedure. The bladder was noted to be friable with erythematous mucosa and there was extravasation of contrast suggesting perforation.
There was mild baseline hyponatremia attributed to cirrhosis. Pre procedure the serum sodium was 133 meq/L. Immediately post procedures it was 122 meq/L. Labs were repeated and the serum sodium continued to drop nadiring at 115 meq/L approximately 6 hours post operatively. There were associated mental status changes, lethargy and confusion.
Two 100 ml boluses of 3% saline given. Serum sodium increased (118 mmol/L – 120 mmol – 122 mmol -125 mmol -127 mmol) over the subsequent 16 hrs.
This was a case of glycine induced translocational hyponatremia. For certain urologic, such as transurethral resection of the prostate (TURP) or transurethral resection of a bladder tumor (TURBT) and (TURP/ TURBT) and gynecology procedures such as hysteroscopy, instillation of fluid is required for distension and irrigation. When certain types of electrocautery are required electrolyte based solutions (such as 0.9% saline) cannot be used as they are conductive.
In these cases non conductive fluids are required. The most common solution used is glycine 1.5%. Under certain conditions the glycine can be absorbed into the circulation. Risk factors include:
- Large volume of solution
- Prolonged procedure
- Vascularity of tissue
- Perforation
In this case the measured serum osmolarity 6 hours post procedure was 282 mOsm/kg confirming isotonic hyponatremia. The calculated osmolarity was 246 mOsm/kg . This osmolar gap indicated the presence of an unmeasured osmole presumed to be glycine.
As this was isotonic hyponatremia one would not expect cellular edema. So, what was the cause of the lethargy and altered mental status?
Glycine is associated with neurologic manifestations by the following mechanisms:
- Glycine itself has neurotoxicity acting as an inhibitory neurotransmitter.
- Glycine is metabolized to ammonia.
In this case the post procedure ammonia was 297. The following morning it had improved to 43 and the mental status changes had resolved.
It is debatable whether 3% saline is necessary or should have been given in these situations as the hyponatremia typically is isotonic or hypotonic. Glycine enters cells, is metabolized and excreted in the urine. Therefore the serum sodium typically increases without treatment.
As these cases are acute hyponatremia (< 48 hrs), rapid correction is acceptable.
In severe cases, especially if associated with AKI, acute hemodialysis may be required. This will correct the hyponatremia and remove glycine and its metabolites.
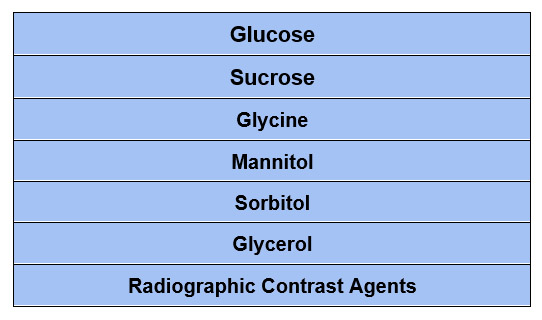
Causes of Translocational Hyponatremia
Summary
The accumulation of an effective osmole can cause hyponatremia by translocation of water from the intracellular to extracellular space. This is commonly seen in severe hyperglycemia. Some less common causes involve sucrose and glycine.