Table of Contents
Thrombotic microangiopathy (TMA) comprises conditions that are of importance to nephrologists as they are:
- Associated with renal manifestations including acute kidney injury
- Frequently require treatment with plasmapheresis, a procedure which is often managed by the nephrologist
Pathophysiology – What is it?
A pathologic condition characterized by platelet microthrombi in the microvasculature. This manifests as:
- Thrombocytopenia
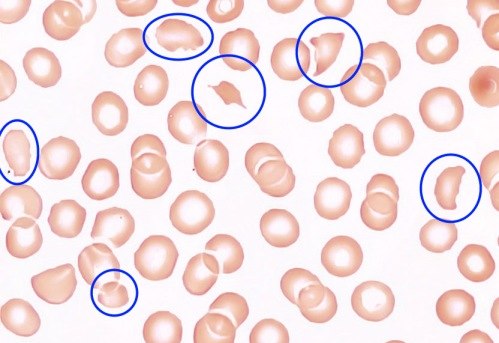
- Microangiopathic hemolytic anemia (Hemolytic anemia caused by mechanical RBC destruction in the microvasculature characterized by schistocytes). This in contrast to autoimmune hemolytic anemia where autoantibodies attack the RBC’s.
- End organ dysfunction (often renal)
Causes of Thrombotic Microangiopathy
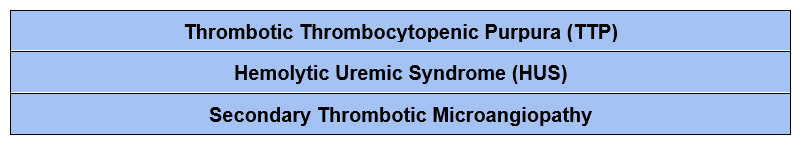
Thrombotic Thrombocytopenic Purpura (TTP)
TTP is a condition where there is a deficiency of a protein called ADAMTS 13
- ADAMTS 13 normally cleaves large vWF multimers into smaller fragments.
- A deficiency of ADAMTS 13 ➔ accumulation of large von Willebrand Factor (vWF) multimers.
- Large vWF multimers ➔ increased platelet binding and thrombi in the microvasculature
➔ clinical manifestations of thrombocytopenia, microangiopathic hemolytic anemia and end organ dysfunction
The deficiency in ADAMTS 13 can be caused by:
- An inhibitory autoantibody
- A hereditary deficiency
There is a classic pentad of clinical manifestations
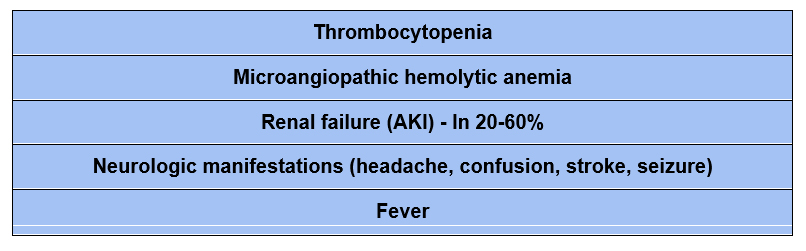
The presence of the full pentad is rare, it is a late manifestation. Often on the dyad of thrombocytopenia and microangiopathic hemolytic anemia are present.
Hemolytic Uremic Syndrome (HUS)
In HUS, the inciting event is damage to endothelial cells.
- Damage to endothelial cells ➔ activation of the coagulation cascade ➔ microthrombi in the microcirculation ➔ similar clinical manifestations as TTP. It is typically divided into diarrheal (dHUS) and atypical (aHUS).
Diarrheal/ Shiga toxin associated HUS (dHUS)
- Shiga toxin (most commonly associated with E coli O157), causes endothelial cell damage.
- Clinical presentation: enterocolitis with bloody diarrhea (in 90%)
Atypical HUS (aHUS)
- Genetic defect of or acquired autoantibody to complement regulatory factors.
- There is constitutive activation of the alternative complement pathway, kept in check by complement regulatory factors.
- A deficiency or impairment ➔ uncontrolled activation of the alternative complement pathway.
- Complement deposition ➔ endothelial cell damage, creating the milieu for microvascular thrombosis.
- Complement regulatory factor abnormalities include:
- Factor H (loss of function)
- Factor I (loss of function)
- C3 convertase (gain of function)
- C4 binding protein (gain of function)
- Complement factor B (gain of function)
- Thrombomodulin (gain of function)
- Membrane cofactor protein (gain of function)
- In up to 1/3 cases of a HUS no complement abnormality can be identified
- Complement regulatory factor abnormalities include:
Classic clinical triad
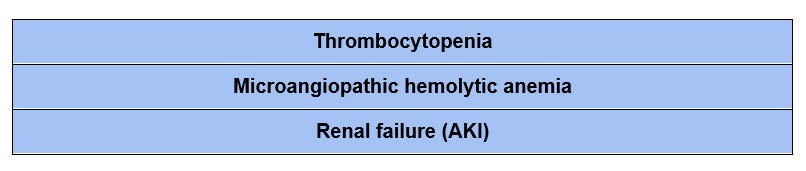
As in TTP only the dyad of thrombocytopenia and microangiopathic hemolytic anemia may be present. Neurologic manifestations can also occur in HUS.
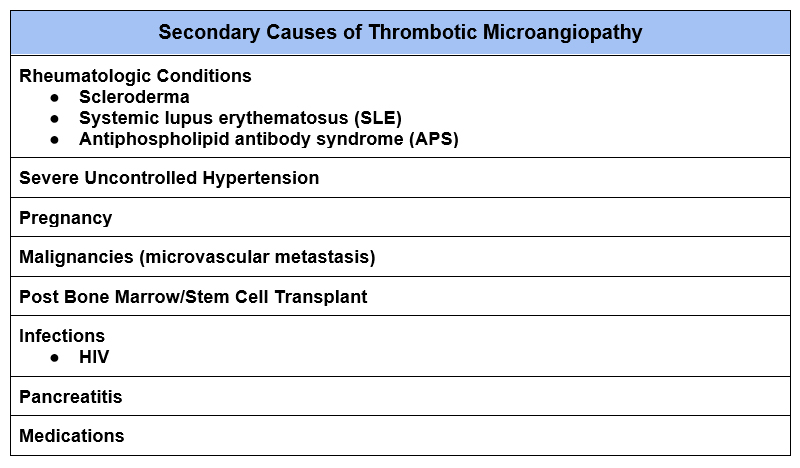
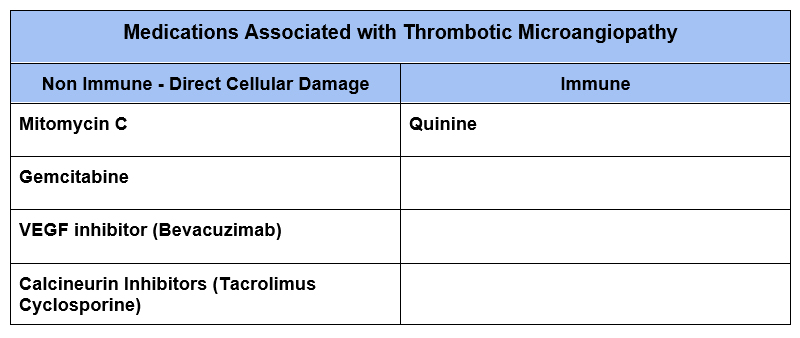
Secondary Thrombotic Microangiopathy
There are a number of systemic conditions and drugs that are associated with microangiopathic hemolytic anemia and thrombocytopenia.
Diagnosis
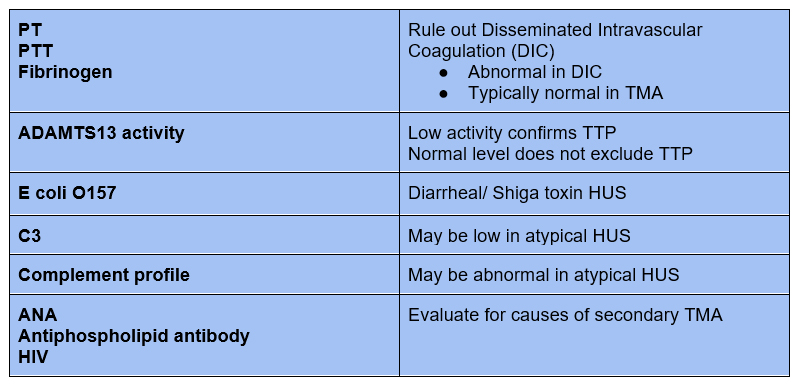
Confirm Thrombotic Microangiopathy
- The clinical dyad of microangiopathic hemolytic anemia and thrombocytopenia are sufficient to diagnose a thrombotic microangiopathy
- To confirm thrombotic microangiopathy check the:
- LDH, typically elevated in TMA (released from destruction of RBCs and tissue ischemia)
- Peripheral blood smear for schistocytes (pathognomonic for microangiopathy)
Clinical Findings:
- In any case of Acute Kidney Injury (AKI), I take a quick look at the hemoglobin and platelet count. If anemia and thrombocytopenia I check the LDH and peripheral smear
- The presence of end organ damage does not distinguish cause
- Kidney Injury more common in HUS, also occurs frequently with TTP
- Neurologic manifestations although classically described with TTP also can occur with HUS
- Bloody diarrhea. Suggests Shiga toxin associated HUS (present in 90%)
Secondary Laboratory Evaluation
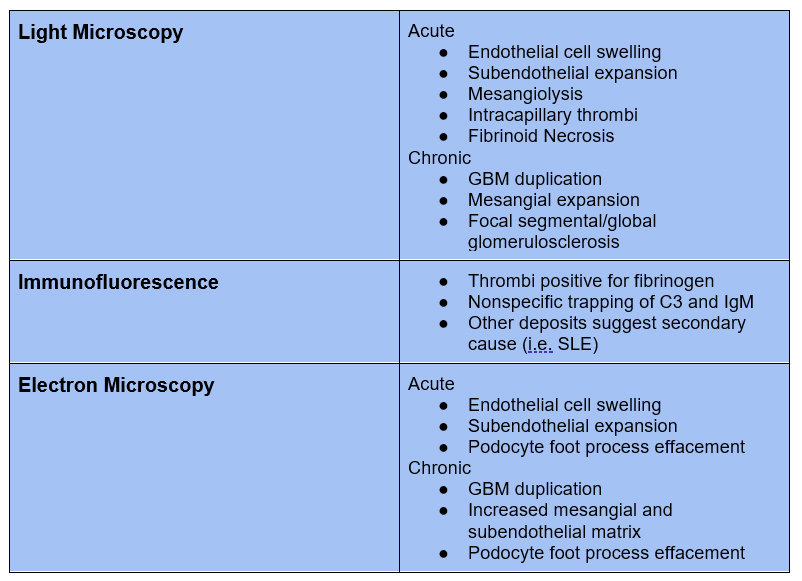
Renal Biopsy
Renal biopsy often is not done given associated thrombocytopenia. Findings typically do not distinguish the underlying cause of thrombotic microangiopathy.
Treatment
These conditions (especially TTP) may have a high mortality. The mortality in TTP without treatment is > 90%
Platelet transfusions are generally avoided in TTP. Bleeding is rare and there is concern that transfusion may exacerbate the condition. A femoral line for pheresis often can be safely done with severe thrombocytopenia. FFP may be transfused for line placement prior to plasmapheresis. Despite this if there is severe bleeding platelets should be given.
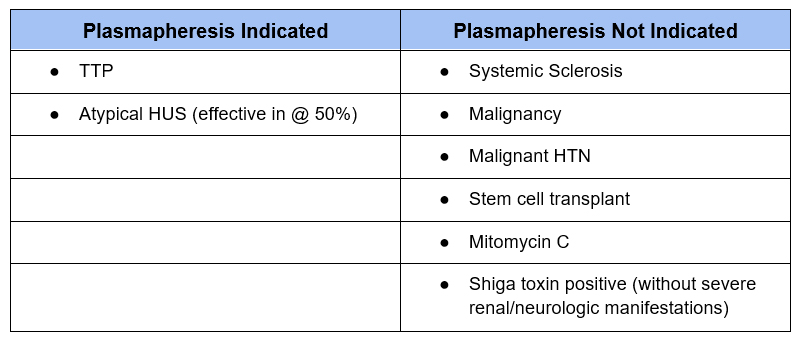
Plasmapheresis
- Performed in most cases initially. Plasmapheresis removes the inhibitory autoantibody and replaces ADAMTS 13 (present in FFP)
- Improves patient survival in TTP to > 80%
- Plasmapheresis done daily with FFP.
- Trend platelet count and LDH (continue if LDH elevated, even if platelet count normal)
- If refractory can use cryosupernatant (the portion of FFP that contains ADAMTS 13) or solvent detergent treated plasma
Glucocorticoids
- Help prevent allergic reactions with plasmapheresis
- Immunosuppressant to decrease autoantibody production
Rituximab
- Used in TTP
- Immunosuppressant to decrease autoantibody production
- Dose: 375 mg/m2 weekly x 4
- Removed by plasmapheresis, hold 1-2 days after rituximab infusion
Eculizumab
- Used in atypical HUS
- Monoclonal antibody to C5
- Blocks C5 activation thereby inhibiting the complement system
- Increased infection risk (require meningococcal vaccination)
Caplacizumab
- May be used in TTP
- Monoclonal antibody against von willebrand factor
- Newer medication (approved in 2019).
- I have not seen it used as of writing this article.
Summary
Thrombotic microangiopathies comprise a range of conditions that cause microangiopathic hemolytic anemia, thrombocytopenia and often acute kidney injury. Treatment for primary causes often includes plasmapheresis with FFP.



