Table of Contents
Here’s my approach to proteinuria.
Albumin, microalbumin, protein – What’s the difference?
- Most urinary protein is albumin
- In glomerular diseases urinary albumin is 55-60% of the total urinary protein
- If the percentage is low (urinary albumin < 40% of the total urinary protein) think tubulointerstitial disease
- If the percentage is very low (urinary albumin < 20% of the total urinary protein) think Bence Jones proteinuria (myeloma)
How do we classify the severity of proteinuria?
Microalbuminuria
-
- Albumin Creatinine ratio: 30- 300 microgram/ mg (or milligram/gram its the same thing)
- Equivalent protein creatinine ratio: 150 – 500 milligram/gram
By the way, they don’t like to call it microalbuminuria any more. They’re worried that people will think micro means “really small” albumin as opposed to what it really means, a really small amount of albumin in the urine. They called it this because it usually wasn’t enough to show up on a urinalysis dipstick. So KDIGO says to call it “moderately increased” albuminuria instead. How they decided what used to be a really small amount is now moderately increased I don’t know.
(KDIGO – Kidney Disease: Improving Global Outcomes. A bunch of experts going around writing guidelines)
Overt Proteinuria
-
- Albumin Creatinine ratio: > 300 microgram/ mg (or milligram/gram its the same thing)
- Equivalent protein creatinine ratio: > 500 milligram/gram
KDIGO calls this “severely increased” albuminuria. Traditionally this was proteinuria that was enough to show up on a urinalysis dipstick. Even though KDIGO uses the above cutoff to call it albuminuria severe, in the real world (at least in the US), above 1000 mg/gm gets a nephrologist’s attention. If we can’t get the proteinuria to less than 1,000 mg/gm most nephrologists will think about a kidney biopsy.
Nephrotic Range Proteinuria
-
- More than 3.5 grams / 24 hrs
- Protein Creatinine ratio > 3500 mg/g, Albumin creatinine ratio >2200 mcg/mg. This is an assumption. More on that below.
This is why I don’t like that KDIGO classifies an albumin creatinine ratio of > 300 as “severely increased”. Nephrotic is severe, it’s not all the same.
Nephrotic proteinuria is more than 3.5 grams per 24 hours, but all I see are protein creatinine ratios and they ran out of those orange jugs. Help!
- Assumption: If the patient peed in the jug for 24 hours there would be 1 gram of creatinine.
- The protein creatinine ratio is reported in milligrams per gram. Using this assumption the ratio (number of milligrams per gram), roughly equals the mg of protein there would be if the patient did a 24 hour urine.
- This assumption is not true because the amount of creatinine in a 24 hour urine depends on muscle mass (an elderly woman may have less 1 gram and a younger muscular man will have more).
- We use this assumption anyway to rate the severity of proteinuria.
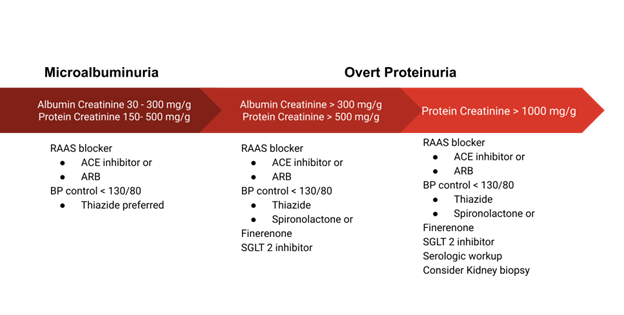
Treatment
- Renin Angiotensin Aldosterone System blockers: ACE inhibitors/ Angiotensin receptor blockers
- Thiazide diuretics
- Mineralocorticoid antagonists
- SGLT 2 inhibitors.
Renin Angiotensin Aldosterone System blockers
Renin Angiotensin Aldosterone System blockers: ACE inhibitors/ Angiotensin receptor blockers:
- 1st line for both overt proteinuria and microalbuminuria.
- Don’t combine these two classes of medications; it’s either one or the other. Combination has been shown to increase adverse events, AKI and hyperkalemia.
- If a patient gets angioedema with an ACE inhibitor, it’s not absolutely contraindicated to use an angiotensin receptor blocker; the cross reactivity percentage is really low.
I usually talk to the patient about it, and find out how severe the reaction was. If it wasn’t severe, I tell them there’s a low percentage of a similar reaction and often give it a try. If the angioedema was severe, I wouldn’t use an ARB. If the angioedema happened with an ARB first, I wouldn’t try an ACE inhibitor.
Thiazide diuretics
Yes, thiazide diuretics. They don’t usually teach this, but it’s true and they’re cheaper than some of the other options. Both in my experience and in this NEJM article they work https://www.nejm.org/doi/full/10.1056/NEJMoa2110730
Look at figure 2A in the above article.
- Lowering BP in general helps lower proteinuria
- A RAAS blocker and thiazide is a synergistic BP lowering combo. In my experience they’re synergistic for proteinuria too.
- If the patient is on an RAAS blocker, BP is not at target and K is mid normal – high, I go this route usually chlorthalidone. In a similar situation, but the K is low normal to low then I use a…
Mineralocorticoid receptor antagonists
Spironolactone is my go to here.
- Not typically taught, but this is my experience and if I looked I’m sure I can find an article to support this.
- I don’t go higher than 25 mg a day if I’m using it for proteinuria or HTN (primary hyperaldosteronism or refractory hypokalemia would be the exception).
- Side effects: hyperkalemia (always check bmp 1-2 weeks after starting) and gynecomastia, usually don’t see that at 25 mg.
Eplerenone
- Supposed to be more specific to mineralocorticoid receptors so it doesn’t cause gynecomastia
- It’s also less potent than spironolactone. I don’t use it much.
Finerenone is the new kid on the block.
- Approved for diabetics (at least when I wrote this). Sure they’ll be looking for (and get) approval for non diabetic CKD.
- Supposedly less prone to hyperkalemia than spironolactone, but still check for it.
- I’ll look to use this in a diabetic with overt proteinuria, already on a full dose RAAS blocker, with BP at or close to target and borderline high potassium. Cost is a consideration here.
SGLT 2 inhibitors
Diabetic med that is licensed for non diabetic CKD. Interesting how it works for proteinuria. RAAS blockers affect the efferent arteriole (leaving the glomerulus), SGLT 2 inhibitors affect the afferent arteriole (entering the glomerulus). Using both together is a cool synergy at least from a physiologic perspective.
- I’m using this in patients who still have overt proteinuria on full dose RAAS blocker and either already on or can’t tolerate chlorthalidone or spironolactone.
- I’m not convinced of benefit (or at least benefit worth the expense or side effects) in CKD patients without proteinuria or with microalbuminuria. See figure 2 in the following article:
https://www.nejm.org/doi/full/10.1056/NEJMoa2204233
The forest plot crosses 1 for those patients.
- I’m also looking for reasons not to use this drug given the adverse effect profile which mainly is UTI’s and fournier’s gangrene. Don’t use it in patients at risk for these.
My Approach
How low do I go?
Microalbuminuria
- Keep it there, prevent it from going to the next range. If I can get it back to normal even better, but I’m not going to go crazy using 3 or 4 different meds to try and do that.
Overt proteinuria
- My goal is to get it less than 300 mcg/mg albumin/500 mg/g protein
- It’s all a continuum lower is better. If I can’t get the protein creatinine ratio less than 500 mg/g I try for less than 1,000 mg/g.
- If nephrotic range, maybe I can’t get the protein creatinine ratio to less than 1,000mg/g. If can decrease it by 50% helped the patient.