Primary hyperaldosteronism is the most common modifiable cause of secondary hypertension with an estimated prevalence as high as 20%.
This article will review normal aldosterone secretion and oversecretion, indications for screening, how to screen and confirm the diagnosis.
Table of Contents
Normal Aldosterone Secretion and Mechanism of Action
- Secreted by the zona glomerulosa of the adrenal gland
- Secretion stimulated by angiotensin II (via activation of the renin angiotensin system)
and elevated plasma potassium.
- Acts on the mineralocorticoid receptor of the principal cell in the distal nephron, increasing activity of epithelial sodium channels (ENaC)
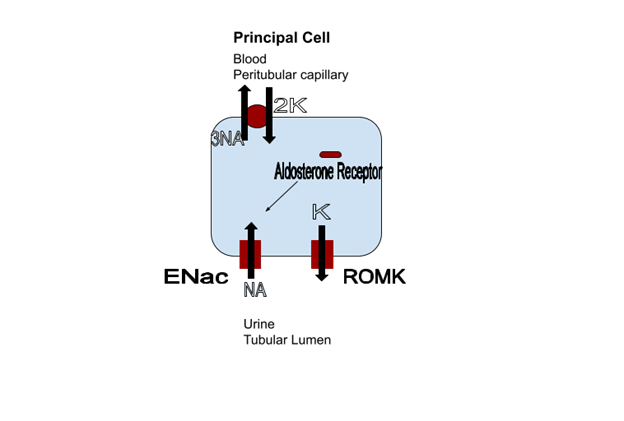
- Increased sodium reabsorption corrects volume depletion and creates an electrochemical gradient for potassium secretion through the ROMK channel, correcting hyperkalemia.
Oversecretion of Aldosterone
Primary hyperaldosteronism is when the adrenal gland secretes aldosterone even when it doesn’t need to (independent of angiotensin II or elevated potassium). This oversecretion can be from an adenoma (which is typically unilateral) or hyperplasia (which is typically bilateral).
- Increased ENaC channel activity from activation of the mineralocorticoid receptor leads to:
- Increased sodium resorption ➞ Hypertension
- Lumen negative electrochemical gradient
➞ Increased potassium secretion ➞ Hypokalemia
- ➞ Increased hydrogen ion secretion ➞ Metabolic alkalosis
- The volume overload then suppresses renin secretion
This causes the classic clinical triad of hypertension, hypokalemia and metabolic alkalosis with a suppressed plasma renin activity.
Although unexplained hypokalemia is a clinical clue to suggest primary hyperaldosteronism, the majority of patients will have normokalemia. The diagnosis should still be considered in hypertension with a normal potassium.
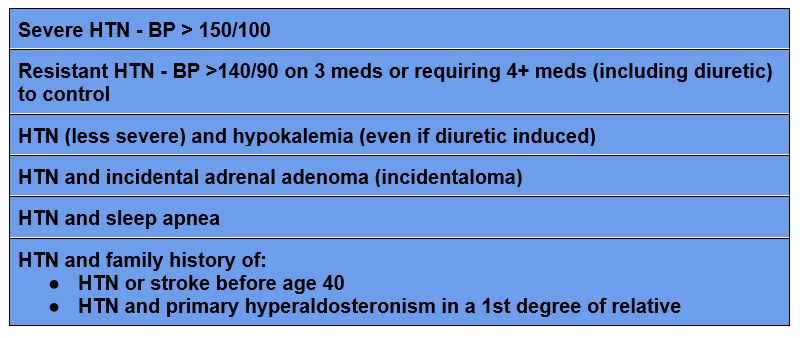
When to Screen for Primary Hyperaldosteronism
Guidelines for screening indications include:
How to Screen for Primary Hyperaldosteronism
Once you have an indication, how do you screen?
The main screening test is the aldosterone renin ratio. This is a plasma (blood) sample for aldosterone and plasma renin activity, typically drawn in the AM with the patient seated.
In primary hyperaldosteronism not only will the aldosterone be high, the plasma renin activity will be suppressed from the volume overloaded state.
An elevated aldosterone ( > 10 ng/dL) with an aldosterone renin ratio of greater than 20 or 30 (depending on reference) is considered a positive screen.
Things to know:
- Both an elevated aldosterone and aldosterone renin ratio are required. This is because the plasma renin activity is typically less than 1, and a denominator less than 1 can drive a high ratio even if the numerator is not very high.
Example:
Aldosterone 5; Plasma Renin Activity 0.1 = ratio of 50
This would not be a positive screen as the aldosterone level is not elevated.
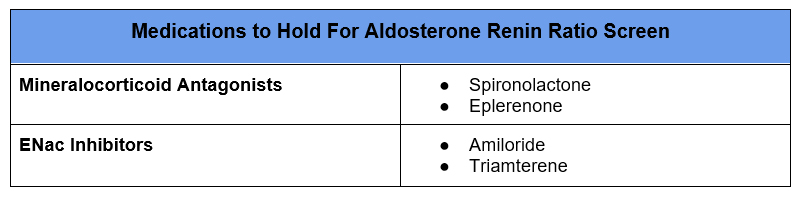
- Certain medications need to be held as they can affect plasma renin activity thereby decreasing the accuracy of this screen. These should be held for 4-6 weeks prior to the screen.
- I typically do not hold renin angiotensin system (RAS) blockers (ACE inhibitors or angiotensin receptor blockers), although they can raise the plasma renin activity and decrease the sensitivity of the screen.
- If both the plasma renin activity and aldosterone are elevated this would be secondary aldosteronism.
Confirming the Diagnosis
The diagnosis is confirmed by determining if it is possible to suppress the elevated aldosterone. The main way to suppress aldosterone is to expand the plasma volume with sodium. There are several ways to do this.
I typically measure a 24 hour urine aldosterone with high sodium intake. Another protocol measures plasma aldosterone after an intravenous saline challenge.
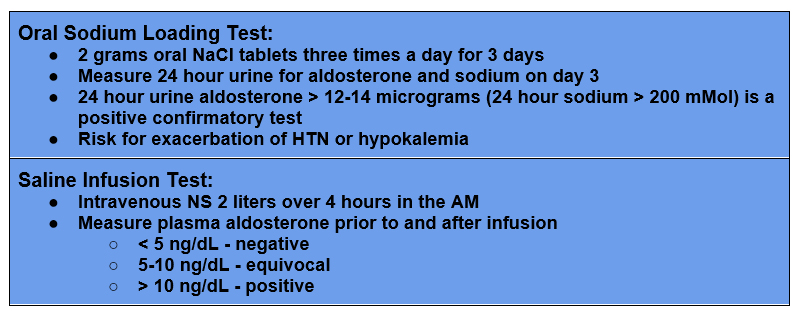
There are two other confirmatory tests described, fludrocortisone suppression and captopril challenge. I have not seen either of these tests performed in clinical practice.
Treatment
There are two methods of treatment for primary hyperaldosteronism:
- Surgical adrenalectomy for unilateral hypersecretion
- Medical (mineralocorticoid antagonist) for bilateral hypersecretion or if the patient is not a surgical candidate.
Adrenalectomy
Laparoscopic adrenalectomy is the preferred treatment with unilateral hypersecretion as it offers a potential for cure and is associated with long term cardiovascular and mortality treatment benefit.
Prior to surgery it is essential to confirm the hypersecretion is unilateral, even if an adenoma is present on imaging, as there is a significant prevalence of non functioning adenomas. This is done by adrenal vein sampling.
This article showed that if the decision for adrenalectomy was made based on imaging it would have been wrong in 37.8% of patients.
- 6% – imaging showed unilateral adenoma and hypersecretion was bilateral
- 1% – imaging showed no abnormality or bilateral hyperplasia and secretion was unilateral
- 9% – imaging showed unilateral adenoma, but hypersecretion was from contralateral adrenal gland.
The exception is if a unilateral adenoma is found in a patient under the age of 35 as non functioning adenomas are rare before this age.
Adrenal vein sampling is a technically difficult procedure as the right adrenal vein is very small and should be done by an experienced interventional radiologist.
Mineralocorticoid Antagonist
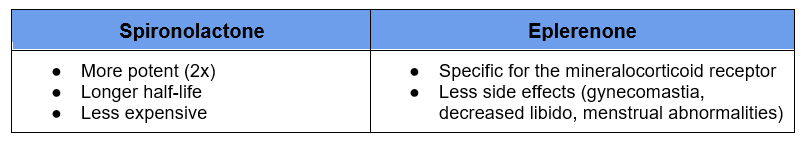
For patients with bilateral hypersecretion, who are not surgical candidates or who decline surgery medical treatment with a mineralocorticoid antagonist is required. There are two medications used spironolactone and eplerenone. Spironolactone is preferred as it is more effective, but has more side effects as it is not specific for the mineralocorticoid receptor.
In addition to controlling the blood pressure and potassium, mineralocorticoid antagonists should be titrated to the plasma renin activity. It has been shown that titration to an increase in the plasma renin activity of > 1.0 ng/ml per hour decreases the risk of cardiovascular events.
If a mineralocorticoid antagonist cannot be tolerated, the second option is to use an epithelial sodium channel (ENaC) blocker such as amiloride.
Summary
Primary hyperaldosteronism is the most common cause of modifiable secondary hypertension. It is often underdiagnosed. Hypokalemia, although common, is often not present. A positive screen requires an elevated aldosterone in addition to a high aldosterone renin ratio. Confirmation requires demonstration that the aldosterone is not suppressible, most often by assessing 24 hour urine aldosterone with high sodium intake. Adrenal vein sampling is required prior to surgery unless there is a unilateral adenoma in a patient under 35.



