Table of Contents
Endocrine disorders are in the differential diagnosis of hyponatremia. These need to be distinguished from SIADH (Syndrome of Inappropriate Antidiuretic Hormone).
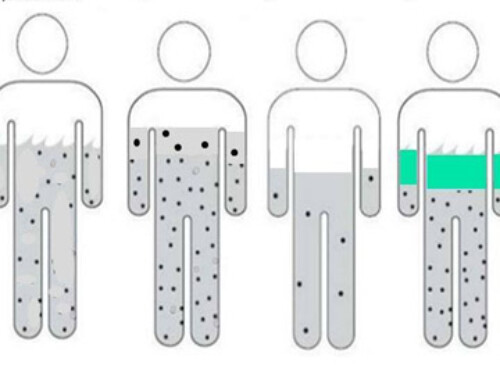
In the article on the laboratory evaluation of hyponatremia read here and watch here, we learned that in hypotonic hyponatremia if the urine osmolarity is > 100 ADH is present and that if the urine sodium is > 40 it is not hemodynamic and therefore inappropriate.
There are additional causes of hyponatremia with these lab findings:
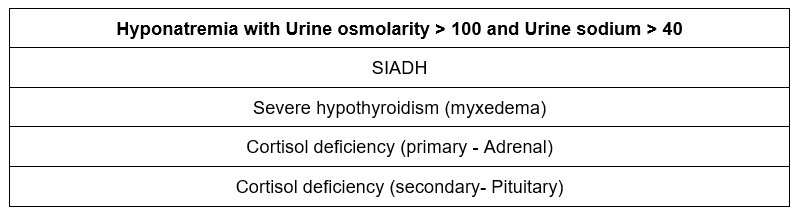
Severe hypothyroidism
I have never seen a case of hyponatremia caused by hypothyroidism. When caused by this it needs to be very severe hyponatremia, like myxedema.
Primary cortisol (adrenal) insufficiency
This is a cause that most are familiar with and is why a morning cortisol +/- cosyntropin (ACTH) stimulation test is often done in the evaluation of hospitalized patients with hyponatremia.
Secondary adrenal (pituitary) insufficiency
A less familiar etiology of hyponatremia is Secondary adrenal insufficiency (secondary to pituitary dysfunction) as a cause of hyponatremia.
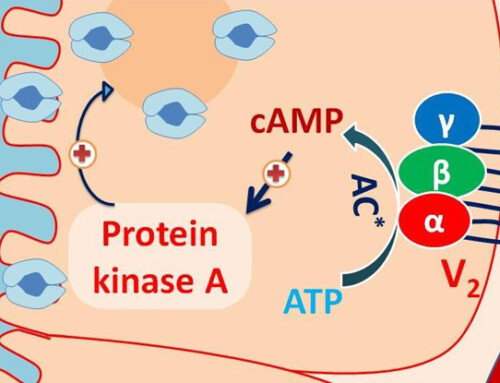
Cortisol suppresses ADH release via a negative bio feedback loop. So cortisol deficiency
- Lack of suppression of ADH
- Hyponatremia that mimics SIADH
Here are 2 stories of hyponatremia caused by pituitary insufficiency:
I had read an article in a European endocrinology journal that described this phenomenon.
European Journal of Endocrinology, Volume 148, Issue 6, Jun 2003, Pages 609–617, Severe hyponatremia due to hypopituitarism with adrenal insufficiency: report on 28 cases in
They recommended the best way to evaluate for this is in a postmenopausal woman with an FSH, follicular stimulating hormone. In a postmenopausal woman the FSH should be high. If it is not high then be suspicious of pituitary dysfunction. If the pituitary insufficiency has not been chronic, it may be missed by a cosyntropin (ACTH stim test), as the adrenal gland may still function well enough to respond to ACTH.
So an FSH has become a part of my evaluation of hyponatremia, specifically in post menopausal women with recurrent hyponatremia. And here is what happened.
Story 1
A woman was hospitalized with recurrent hyponatremia. This was attributed to HCTZ which was discontinued during a prior hospitalization with improvement in the hyponatremia. She was rehospitalized with recurrent hyponatremia, off of HCTZ when I saw her. The FSH was not elevated leading me to be suspicious of pituitary dysfunction. However, she was in a perimenopausal age range, so I went back to ask her if she still had her periods. Her answer, “I haven’t had a period since I hurt my head in a car accident 20 years ago”.
What happened was this. After her car accident she was treated with a nasal spray (this would have been ddavp). This was central diabetes insipidus due to trauma to the posterior pituitary. After some time she was told she did not need the ddavp nasal spray anymore. She had developed anterior pituitary insufficiency with amenorrhea as well as ACTH and secondary cortisol deficiency presenting as recurrent SIADH.
Of course, a better way to make this diagnosis may have been to elicit the history first, then do the confirmatory lab testing. But, that is how this diagnosis was made.
Story 2
A Brazilian woman was hospitalized in the ICU with severe hyponatremia. I can’t remember if her cortisol and cosyntropin stimulation test were off or if it was the FSH that was inappropriately low. In any event we learned through the Portuguese translator that she had never been the same, never felt right after she gave childbirth in rural Brazil. There had been significant postpartum bleeding. She had gone to doctors in Brazil prior to coming to the United States, but no one was able to figure out the cause of her symptoms.
She had Sheehan syndrome (pituitary infarction), which is described with severe postpartum hemorrhage causing hypotension. It ultimately results in a small pituitary giving the appearance of an “empty sella”.
Both of these patients did well with hormonal treatment including maintenance doses of hydrocortisone.
Summary
Pituitary causes of hyponatremia do occur. Although in these cases the history was elicited in retrospect, it does highlight how cortisol/cosyntropin stimulation test and an FSH (in postmenopausal woman) along with a high index of suspicion can elicit this diagnosis.
Secondary cortisol (pituitary) insufficiency:
- Mimics SIADH, euvolemic with urine osmolarity > 100 and urine osmolarity > 40
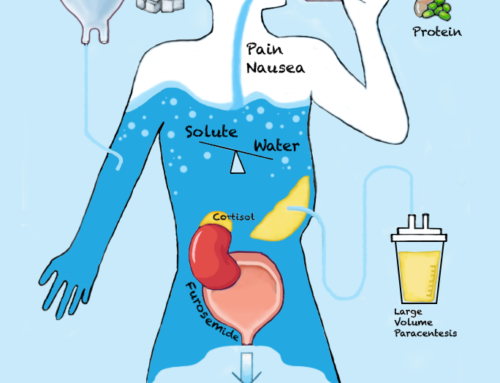
- Symptoms may be similar to SIADH (nausea/ vomiting; confusion)
- May have findings of deficiency of other pituitary hormones (pale/doughy skin; scant pubic/axillary hair)
- Hyperkalemia not present (aldosterone intact)
- Low cortisol, may or may not have appropriate response to cosyntropin stimulation test, depending on chronicity
- FSH inappropriately low in postmenopausal women