Table of Contents
The definition of dialysis is: “the separation of particles in a liquid on the basis of differences in their ability to pass through a membrane”.
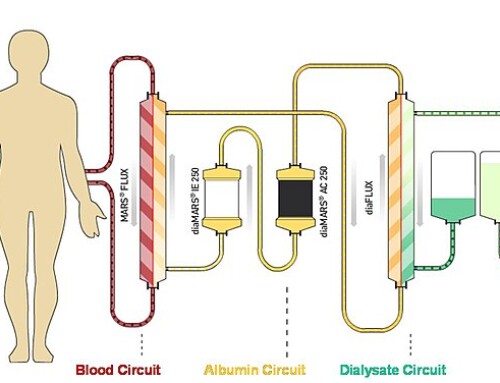
Clinically dialysis requires:
- Access to blood
- A semipermeable membrane
- Dialysis solution
Particles (urea, creatinine, other uremic molecules and electrolytes) diffuse between blood and dialysate down the concentration gradient.
For hemodialysis the semipermeable membrane is a synthetic hemofilter also referred to as a dialyzer.
The peritoneum is a membrane that lines the abdominal cavity. It is highly vascular with many capillaries allowing it to serve as the semipermeable membrane for peritoneal dialysis.
Requirements for Dialysis
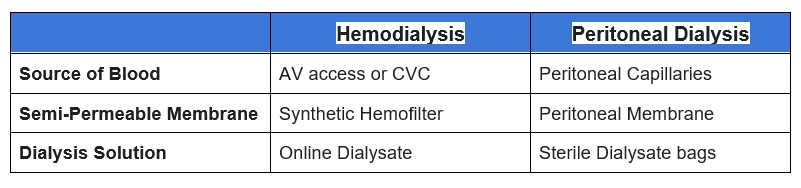
Differences between Hemodialysis and Peritoneal Dialysis.
The mechanism of diffusion of uremic molecules and electrolytes is similar for both hemodialysis and peritoneal dialysis. However, there are some important differences.
- Membrane
- Peritoneal membrane is permeable to protein, the hemodialysis membrane is not.
- Fluid removal (ultrafiltration)
- Hemodialysis: Hydrostatic pressure, specific volume can be achieved
- Peritoneal Dialysis: Oncotic pressure, variable volume
Peritoneal Dialysis typically contains dextrose which serves as the oncotic stimulus for ultrafiltration. This process is similar to what occurs in severe hyperglycemia where fluid (water) moves from the intracellular to extracellular space to equalize the osmotic gradient.
Higher concentration dextrose dialysate is used to obtain higher degrees of ultrafiltration.
With extended dwell times dextrose can be absorbed from the dialysate into the blood causing a decrease in the oncotic stimulus and impairing ultrafiltration. For this reason icodextrin can be used for longer dwells. Icodextrin is a glucose polymer that induces ultrafiltration and is poorly absorbed into the circulation.
Peritoneal Dialysate solutions. Bags are color coded and patients may be more familiar with the color the concentration
- 1.5% Dextrose – yellow
- 2.5% Dextrose – green
- 4.25% Dextrose – red
- 7.5% Icodextrin – purple
Although 4.25% dialysate can induce greater ultrafiltration the high dextrose concentration can be toxic to the peritoneum. For this reason its use should be minimized.
How is Peritoneal Dialysis Performed?
There are three steps of peritoneal dialysis
- Fill – dialysate is instilled into the peritoneal cavity
- Dwell – dialysate remains in the peritoneal cavity to allow diffusion and ultrafiltration to occur.
- Drain – dialysate is drained and discarded. Fresh dialysate is instilled for the next fill.
Types of Peritoneal Dialysis
The process of dwell, fill and drain can be performed manually or by a machine called a cycler.
- CAPD – Continuous Ambulatory Peritoneal Dialysis
- Manual exchanges typically 4 per 24 hour period, every 4-6 hours during the day with a longer dwell overnight
- CCPD – Continuous Cycling Peritoneal Dialysis
- Machine dwells typically 4-6 over 8-10 hours overnight with a last fill that stays in during day, instilled before disconnecting from machine
- NIPD – Nocturnal Intermittent Peritoneal Dialysis
- Machine dwells typically 4-6 over 8-10 hours overnight without a last fill. Referred to as “dry day”
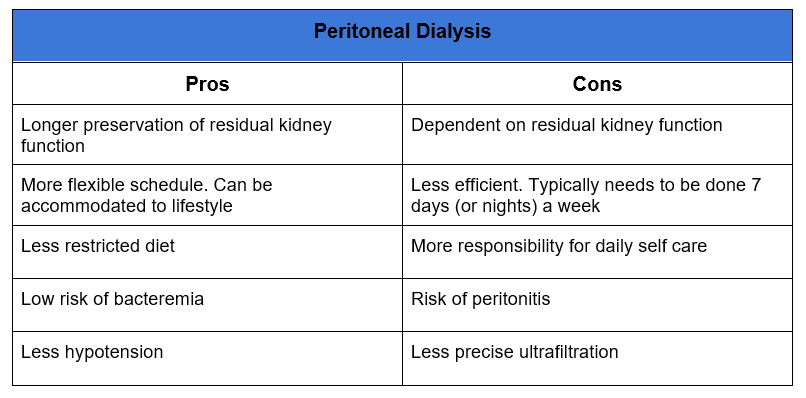
Which is Better: Hemodialysis or Peritoneal Dialysis?
There is no significant mortality difference between Hemodialysis and Peritoneal Dialysis. There may be a slight benefit with PD initially which dissipates over time.
Therefore, patient preference is a major factor.
Things to Know about Peritoneal Dialysis
- Residual kidney function
Peritoneal Dialysis (PD) is often dependent on residual kidney function. When assessing adequacy both the clearance of PD and residual kidney function is taken into account. If residual kidney function is lost PD alone may be insufficient to prevent uremia or the burden of therapy may become too onerous, requiring both the cycler overnight and multiple manual exchanges during the day. For this reason care should be taken to avoid nephrotoxins and preserve residual kidney function in patients on PD.
- Hypokalemia
PD is efficient at potassium removal. Unlike hemodialysis where there is a tendency toward hyperkalemia, it is not unusual for patients on PD to have low potassium requiring supplementation. Potassium can be added to the dialysate, however it is more common to prescribe oral supplementation.
- Protein Losses
The peritoneal membrane is permeable to protein and amino acids. Up to 6-12 grams can be lost daily. Therefore there is a high incidence of malnutrition. Attention needs to be paid to diet and supplementation.
Summary
Peritoneal Dialysis is an ideal modality for renal replacement therapy for many patients offering the benefits of home treatment that can be performed overnight and preservation of residual kidney function. It utilizes the peritoneal membrane for diffusion and ultrafiltration between blood and dialysate.