Table of Contents
NSAIDS are known to be nephrotoxic.
- 1-5% of NSAID users have an adverse kidney event
- Patients with kidney disease are often advised to refrain from NSAIDS.
The thing is NSAIDS work. I’m a nephrologist who takes NSAIDS while advising my patients with CKD to avoid them. What gives?
I recently was asked what stage of kidney disease, what GFR is an absolute contraindication to NSAIDS. I did not have a straightforward answer to this question. After researching and seeking expert opinion I can offer the following considerations:
This article will address some of the adverse renal effects of NSAIDs including
- Acute Kidney Injury (AKI)
- Proteinuria and the Nephrotic Syndrome
- Chronic Kidney Disease (CKD)
- Electrolyte Disorders, particularly hyperkalemia
- Hypertension (HTN) and fluid retention
The renal effects apply to selective COX2 inhibitors as well. These have been considered “safe”, however the safety applies to GI, not renal (or cardiovascular) toxicities.
How NSAIDS affect the Kidney
NSAIDS affect the production of cyclooxygenase. Cycloxygenase is necessary for the conversion of arachidonic acid to prostaglandins. Most of the renal effects of NSAIDS are related to a decrease in prostaglandins. Renal prostaglandin production is impaired by both non selective NSAIDS and selective COX 2 inhibitors.
Renal effects of prostaglandins include:
- Dilation of the afferent arteriole (entering the glomerulus)
- Production of renin
- Renal sodium excretion (natriuresis)
- Decrease in the effect of antidiuretic hormone (ADH)
Acute Kidney Injury
NSAIDS (current use) double the risk of AKI
Hemodynamic AKI
The main mechanism of NSAID induced AKI is hemodynamic related to a decrease in renal perfusion pressure.
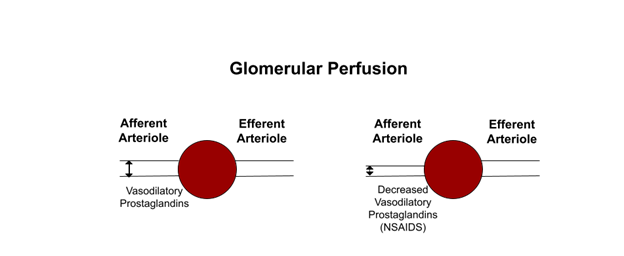
Prostaglandins work to dilate the afferent arteriole, entering the glomerulus. This is a compensatory mechanism to maintain glomerular perfusion pressure and glomerular filtration rate (GFR) when there are other conditions affecting glomerular perfusion.
NSAID associated AKI is therefore more likely in situations where the patient is prostaglandin dependent, that is there is something else going on making afferent arteriole dilatation necessary to maintain glomerular pressure. These include:
- Volume depletion
- Heart Failure
- Cirrhosis
- Renin angiotensin system (RAS) blockers which impair constriction of efferent arteriole, the other compensatory mechanism to maintain glomerular perfusion pressure
- Diuretics
Hemodynamic AKI can be functional, that is resolve upon discontinuation of the NSAID or can ischemic ATN if the decreased perfusion is prolonged and/or more severe.
Chronic kidney disease and age are also risk factors for NSAID associated AKI.
Allergic Interstitial Nephritis (AIN)
Like many medications NSAIDS can cause acute interstitial nephritis.
The interstitial nephritis caused by NSAIDS is unique as it is associated with significant, often nephrotic proteinuria with a minimal change lesion on biopsy.
NSAID induced interstitial nephritis is characterized by:
- Severe AKI
- Abnormal UA (hematuria, pyuria with WBC casts, proteinuria)
- Absence of fever, rash, eosinophilia
- Biopsy:
- Interstitial T cell infiltrate
- Minimal change pathology, normal glomeruli on light microscopy, diffuse foot process effacement on electron microscopy
CKD
The data around NSAIDS and CKD is not as clear. The main reason to avoid NSAIDS in CKD is that CKD increases the risk for AKI
Do NSAIDS cause CKD?
Analgesic Nephropathy
Analgesic nephropathy is a cause of CKD.
- Associated with renal papillary necrosis and calcification.
- Developed in patients who used multiple analgesics combinations chronically and particularly those containing phenacetin. Given this association
- Phenacetin was banned by the FDA in the 1980s.
- Rarely (if ever) seen currently.
Other Association with NSAIDS and CKD
Aside from this there is not good evidence that NSAIDS cause CKD
Nurses health study:
- Higher lifetime NSAID use was not associated with renal function decline.
- Higher lifetime acetaminophen use (cumulative dose 3000 grams or more) was associated with an increased risk of eGFR decline.
Physicians health study:
- Moderate lifetime NSAID use (cumulative dose > 2500 pills) was not associated with an increased risk for reduced creatinine clearance (< 55 ml/min).
- This study did not find an association between acetaminophen and reduced creatinine clearance.
Analgesic Use and Renal Function in Men | Nephrology | JAMA.
Do NSAIDS cause progression of CKD?
Again there is not a lot of good data here. I found one study that showed an increased rate of rapid GFR decline > 15 ml/ minute over a median of 2.75 years (13.3% of patients)
NSAID Use and Progression of Chronic Kidney Disease – The American Journal of Medicine
- Elderly pts (>66) with a baseline eGFR of 60-89 ml/min
- COX 2 inhibitors 25% increased risk (OR 1.25)
- NSAIDS 29% increased risk (OR 1.29)
- Not seen with baseline eGFR < 60 ml/min.
- Higher doses were associated with an increased risk of rapid decline. High dose defined as >90th percentile.
- Celecoxib 120 mg/ day
- Naproxen 300 mg/ day
- Diclofenac 60 mg/ day
- Ibuprofen 700 mg/day
However as eGFR normally decreases with age one can argue that people over the age of 66 with an eGFR 60-89 do not have CKD, but a normal age associated decrease in eGFR. This is one of the reasons that an eGFR of < 60 is used as the cutoff for determining CKD in the absence of other evidence of kidney damage (such as proteinuria).
What? I have Stage 3 Kidney Disease!! Talking to patients about GFR and CKD | BCNephro
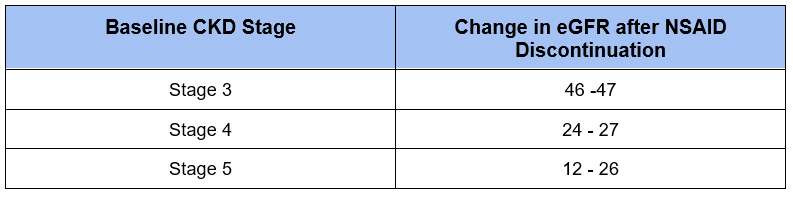
CKD as a risk factor for NSAID induced AKI
Patients with CKD are considered to be at an increased risk of AKI with NSAIDS. As these patients have decreased renal reserve episodes of AKI may contribute to progression of CKD.
Data supporting this come from a study showing the change in eGFR after discontinuation.
Nephrotic Syndrome
Minimal Change Disease
The interstitial nephritis caused by NSAIDS is classically a nephrotic syndrome with minimal change findings on renal biopsy. NSAIDS can also be associated with minimal change disease alone, without the concomitant interstitial nephritis.
Membranous nephropathy
NSAIDS have also been implicated as a secondary cause of membranous nephropathy. There are the classic associated subepithelial deposits. Immunofluorescence stains for IgG1 as opposed to IgG4 in idiopathic primary membranous nephropathy.
Although there are rare case reports of PLA2R antibody positivity in NSAID associated membranous nephropathy, this is generally considered to be indicative of primary/ idiopathic membranous nephropathy. The target antigen in NSAID associated membranous nephropathy is thought to be proprotein convertase subtilisin/kexin type 6 (PCSK6).
Hypertension
Prostaglandins enhance renal sodium excretion:
- Impair sodium resorption in the loop of henle and cortical collecting tubule
- Mediate effects of natriuretic peptides
NSAIDS therefore can contribute to sodium retention contributing to HTN and edema.
Electrolyte abnormalities
Hyperkalemia
- Prostaglandins increase renin secretion and enhance angiotensin II induced aldosterone release
- NSAIDS therefore impair the renin-angiotensin-aldosterone system (RAAS) axis, increasing the risk for hyperkalemia
- Effect seen with other conditions that impair the RAAS axis or renal potassium excretion
- Renin angiotensin system blockers (ACE-inhibitors, Angiotensin receptor blockers)
- Mineralocorticoid antagonists
- Potassium sparing diuretics
- TMP-SMX
- Diabetes
- CKD
Hyponatremia
- Prostaglandins antagonize the effect of antidiuretic hormone (ADH)
- NSAIDS therefore allow for increased ADH effect contributing to hyponatremia risk
Summary
What is the bottom line?
1. It is generally not a good idea to use NSAIDS with:
- Advanced CKD (Stage 4 or 5)
- Propensity toward hyperkalemia
- Hypovolemia
- Cirrhosis or Heart Failure
2. If NSAIDS cannot be avoided, that is the other therapeutic options are worse, then:
- Use the lowest possible dose for the shortest period of time (i.e. < 5-7 days) for acute, or limit use to intermittent for chronic use.
- Reserve for more severe breakthrough pain, utilizing other measures for baseline less severe pain
- Give consideration to holding other medications (RAS blockers, mineralocorticoid antagonists) while NSAIDS are used
- Hold NSAIDS if there is an acute severe dehydrating illness (i.e. gastroenteritis)
- Monitor serum creatinine and electrolytes in @ 1 week and then quarterly. Discontinue immediately if any significant increase in creatinine or potassium.
3. Give consideration to withdrawing NSAIDS with:
- Nephrotic syndrome
- Hypertension
4. Do not use NSAIDS in AKI



