Table of Contents
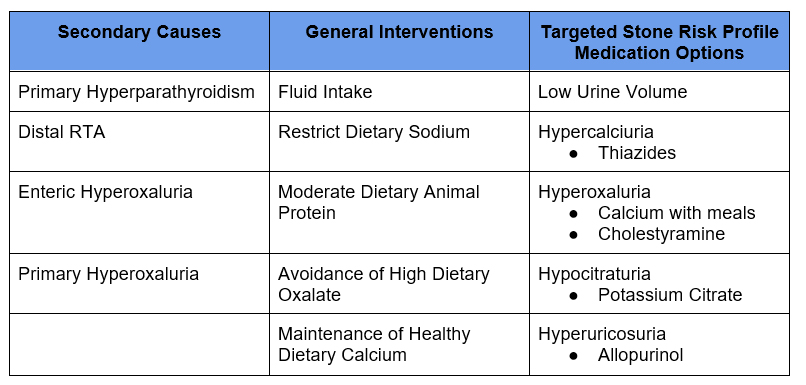
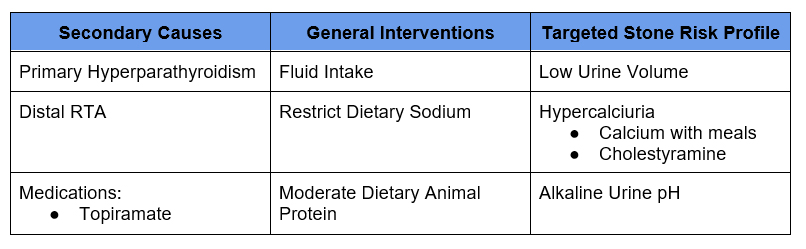
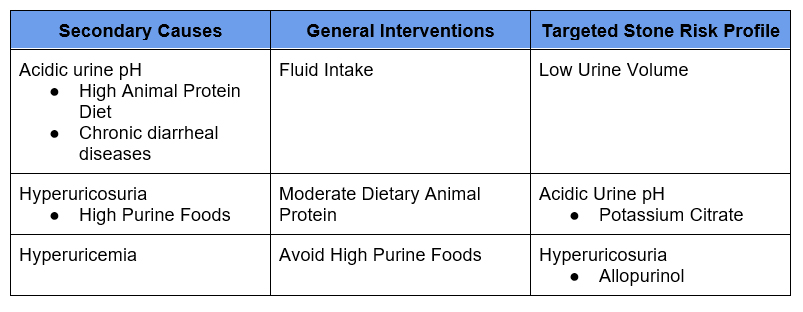
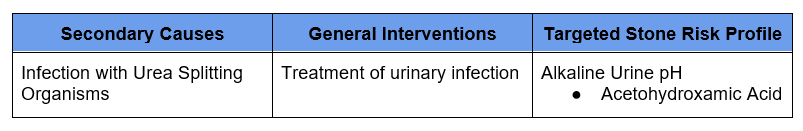
Treatment of Kidney Stones. Once we know or deduce the type of kidney stone, the next focus is treatment. In a patient with recurrent nephrolithiasis, treatment is secondary prevention. That is prevention of stone growth or new stone forming.
Acute stones that are passing are typically managed by urology as they may require surgical intervention. Medical expulsive therapy with alpha blockers (such as tamsulosin) may aid in passage of distal ureteral stones < 10 mm.
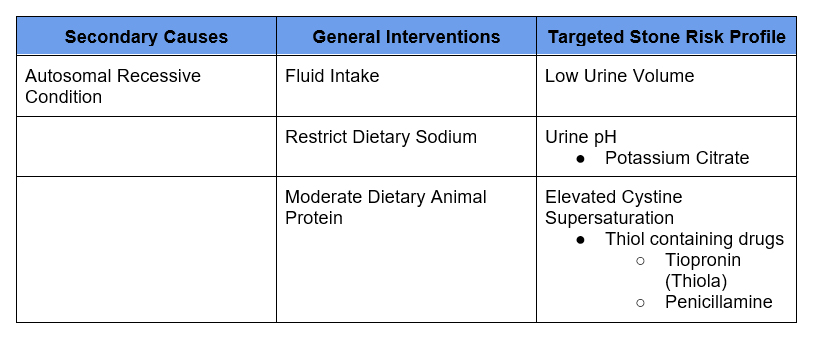
My three prong approach to prevention of recurrent stones
- Rule out secondary causes of stones
- General Dietary interventions.
- Specific interventions (dietary or medication) tailored to patients specific risk factors based on 24 hour urine stone risk profile.
Rule Out Secondary Causes
- Most Common Secondary Causes of Stones
- Primary Hyperparathyroidism
- Distal Renal Tubular Acidosis (Type 1 RTA)
- Enteric Hyperoxaluria
- Medications
- Topiramate
- Calcitriol
- My Screening Evaluation
- BMP +/- Ionized calcium
- PTH
- Phosphorus
- Uric Acid
- Urinalysis +/- Culture
Check out this article for more information – Nephrolithiasis – Approach to Diagnosis of Kidney Stones | BCNephro
General Dietary Interventions
Fluid Intake
Type of Stones:
- Calcium Oxalate
- Calcium Phosphate
- Uric Acid
- Struvite
- Cystine
The most important dietary intervention is fluid intake. The general recommendation is to drink enough fluid to achieve a urinary volume of at least 2 liters a day (2 ½ liters is even better). Since all fluid taken in is not excreted in the urine (the body uses fluid in other ways), I recommend a target of 2 ½ liters intake to achieve a urinary volume of at least 2 liters.
- I recommend water. If someone wants to flavor the water that’s fine, but I don’t believe anything is better than water.
- Some recommend citrus drinks (lemonade, orange juice), but these contain a nominal amount of citrate and typically have a lot of sugar.
- Avoid sodas, they increase the risk of stones.
- For patients with high urinary oxalate, teas should be avoided.
- I counsel patients by advising fluid/water intake in ounces. 240 ml is approximately 8 ounces. I advise 80 ounces (@ 2 ½ liters). Standard water bottles/ containers are 16, 20, or 32 ounces allowing patients to have a target # of water bottles daily.
Restrict Dietary Sodium
Type of Stones:
- Calcium Oxalate
- Calcium Phosphate
- Cystine
I advise this as the second most important dietary intervention. Reducing urinary sodium decreases both hypercalciuria and urinary cystine in cystinuria.
- Recommendation < 100 mmoles (2.3 grams) daily
- High urinary sodium increases contributes to hypercalciuria
- I counsel patients:
- When sodium passes through the kidneys it “drags” calcium with it,
- The only way to reduce sodium in the urine is to reduce how much is taken in
- The majority of sodium (⅔ – ¾ ) is already in food. It requires paying attention to labels and limiting processed foods.
Moderate Dietary Animal Protein
Type of Stones:
- Calcium Oxalate
- Calcium Phosphate
- Uric Acid
- Cystine
This is a secondary dietary intervention. Reducing urinary protein decreases hypercalciuria and urinary cystine in cystinuria. High dietary animal protein is associated with a low urine pH, the main risk factor for uric acid stones.
- Recommendation limit to 0.8-1.0 g/kg day
- Urinary protein metabolites also contribute to hypercalciuria
- I counsel patients:
- It is all forms of animal protein, not just red meat
- Focus on moderation/portion control.
Avoid High Oxalate Foods
Type of Stones:
- Calcium Oxalate
The majority of urinary oxalate comes from endogenous production, not dietary sources. In addition the dietary sources of oxalate tend to be healthier in general. For these reasons the benefits of dietary oxalate restriction are limited.
- High oxalate foods may increase urinary oxalate, there is a floor of which further decreasing oxalate will not be of benefit,
- I counsel patients to avoid very high oxalate foods (or if taken do so in moderation with an extra glass of water). These include:
- Spinach and other leafy green vegetables
- Rhubarb
- Certain nuts
Maintain Healthy Dietary Calcium
Type of Stones:
- Calcium Oxalate
Although counterintuitive dietary calcium restriction paradoxically increases the risk of calcium stones. It does this by allowing more dietary oxalate to be absorbed.
Comparison of Two Diets for the Prevention of Recurrent Stones in Idiopathic Hypercalciuria | NEJM
- Recommend 1000-1200 mg of dietary calcium daily
- Recommend against calcium supplements as they are more absorbed. If absolutely necessary recommend:
- Take with largest meal
- Calcium citrate as opposed to calcium carbonate
- If needed for bone health acceptable to take Vitamin D3
Diet High in Fruits in Vegetables
Type of Stones:
- Calcium Oxalate
- Calcium Phosphate
- Uric Acid
- Struvite
- Cystine
A diet high in fruits and vegetables with high dietary potassium are associated with increased urinary citrate and a decreased incidence of kidney stones.
24 hour Urine Stone Risk Profile: Targeted Approach
Stone risk profiles will provide supersaturations for calcium oxalate, calcium phosphate and uric acid as well as a cystine screen. These provide an overall assessment of stone risk. Elevated supersaturations will indicate a need for therapy. The individual components (listed below) will guide which specific dietary and medication therapies will be of greatest benefit.
Volume
- Low urine volume increases risk for all stone types.
- Target urine volume
- > 2.0 – 2.5 liters most stones
- > 3.0 liters cystinuria
- Treatment
- 8 ounces additional fluid (water) for every 250 ml below target urine volume
Calcium
- Hypercalciuria increases risk for calcium oxalate and phosphate stones
- If elevated look at sodium and protein metabolites to assess if further diet restrictions possible,
- Treatment
- Thiazide diuretic
- If hypokalemia requiring potassium sparing diuretic use amiloride as triamterene can cause drug stones.
Oxalate
- If normal < 40 can advise patients oxalate restriction not as necessary and they can focus diet efforts in other areas.
- Modest increases may benefit from dietary restriction.
- Severe elevations > 100 suggest possibility of primary or enteric hyperoxaluria
- Treatment
- Calcium with meals
- Cholestyramine
- Avoidance of Vitamin C. Vitamin C increases endogenous oxalate production
Citrate
- Citrate is a stone inhibitor. Hypocitraturia increases risk of calcium stone
- Low urine citrate may be associated with RTA (high urine pH) or diarrheal diseases (low urine pH)
- Treatment
- Potassium Citrate (or potassium bicarbonate)
- Sodium citrate or sodium bicarbonate alternative, but less preferred as sodium may increase hypercalciuria.
- Use cautiously with calcium phosphate stones as these may also increase urinary pH
pH
- pH < 5.5 increases risk for uric acid stone
- pH > 6.3-6.5 increases risk for calcium phosphate stones
- pH > 7.5 associated with struvite stones
- Treatment (Uric acid low pH)
- Potassium Citrate (or potassium bicarbonate) Target pH > 6.5
- Treatment (Uric acid low pH)
- Potassium Citrate (or potassium bicarbonate) Target pH > 7
- Treatment (Struvite high pH)
- Acetohydroxamic Acid
Sodium
- High urine sodium risk contributes to hypercalciuria and urinary cystine.
- Target < 100 mmol (2.3 grams day). (Molecular weight of sodium is 23)
Protein Metabolites
- Contributes to hypercalciuria and urinary cystine.
- If elevated, advise moderation of animal protein.
Uric Acid
- Main risk factor for uric acid stones is low urine pH not hyperuricosuria
- Elevation may be a risk factor for calcium oxalate stones, by providing a nidus for calcium crystallization to occur.
- Consider allopurinol or other xanthine oxidase inhibitor
- Uric acid stones: If elevated and/or gout or recurrent stones despite urinary alkalinization
- Calcium oxalate stones: If elevated
Prevention Based on Stone Type
Calcium Oxalate
I counsel patients that calcium stones cannot be dissolved by medical therapy. The nonobstructing stones that are present will either stay (most often not causing a problem) or pass. I have not been able to figure out what makes them pass.
Calcium Phosphate
Like Calcium Oxalate, Calcium Phosphate stones cannot be dissolved by medical therapy. Look for secondary causes of an alkaline urine pH > 6.3-6.5
Uric Acid
The main risk factor is an acidic urine pH < 5.5. Uric acid stones can be dissolved with urinary alkalinization.
- High animal protein diet and chronic diarrheal diseases are causes of low urine pH
- Mainstay of treatment is urinary alkalinization
- Potassium Citrate (Urocit K; Theralith) preferred.
- Sodium Citrate or Sodium Bicarbonate will also alkalanize urine, but not preferred given sodium load.
- Alopurinol can be added if hyperuricemia, hyperuricosuria
Struvite
These are infection stones. The main risk factor is infection with urea splitting organisms, Proteus, Klebsiella. These stones need to be surgically removed with antibiotic treatment to eliminate any nidus for infection.
Cystine
Cystinuria is an autosomal recessive condition. This condition is difficult to treat and is associated with frequent recurrence. Target very high urine volume > 3 liters per day and urine pH > 7. Thiol binding drugs are often required. These have a number of potential side effects including cytopenias, hepatotoxicity and proteinuria. Monitoring of CBC, LFT’s and urine protein is required.
Summary
Prevention of kidney stones requires identifying and treating any secondary causes as well general interventions based on stone type including high fluid intake and dietary sodium restriction. 24 hour urine stone risk profile is key as it allows targeted dietary and medication prescription and monitoring of therapy.



