Table of Contents
MPGN is not a specific disease, it is a pattern of injury seen on light microscopy of kidney biopsy.
- Membrano – Diffuse thickening of glomerular capillary walls
- Proliferative – Increased number of cells in the glomeruli
Therefore MPGN is when glomeruli have both thickened capillary walls and an increased number of cells.
This article will discuss:
- Clinical Presentations
- Classification
- Etiologies
- Evaluation
- Treatment
Clinical Presentations
There are a wide range of clinical presentations including:
- Proteinuria (nephrotic or subnephrotic)
- Nephritic – glomerular hematuria with variable degrees of proteinuria, with or without abnormal or worsening kidney function
- Systemic vasculitic syndrome
Classification
Traditional classification – Electron Microscopy
When I was a nephrology fellow classification was based on the type of immune complexes seen on kidney biopsy electron microscopy.
Type I – Subendothelial and mesangial deposits (Ig and C3)
Type II – (Dense Deposit Disease) – intramembranous deposits
Type III – Both subepithelial and subendothelial deposits
Tip:
In general subendothelial deposits are worse (they are more likely to cause inflammation with a nephritic picture with worsening kidney function) than subepithelial deposits (which are seen in membranous nephropathy) and mesangial deposits (which are seen in IgA nephropathy)
The traditional classification was based on where the immune complex deposits are, not what caused them.
We want to know the underlying cause of the immune complexes that are causing the kidney disease. It’s all about the immunofluorescence.
Pathophysiology of the immune complexes – Immunofluorescence
They can be caused by:
- Immune complex deposition
- Monoclonal immunoglobulin deposition
- Dysregulation of the alternative complement pathway
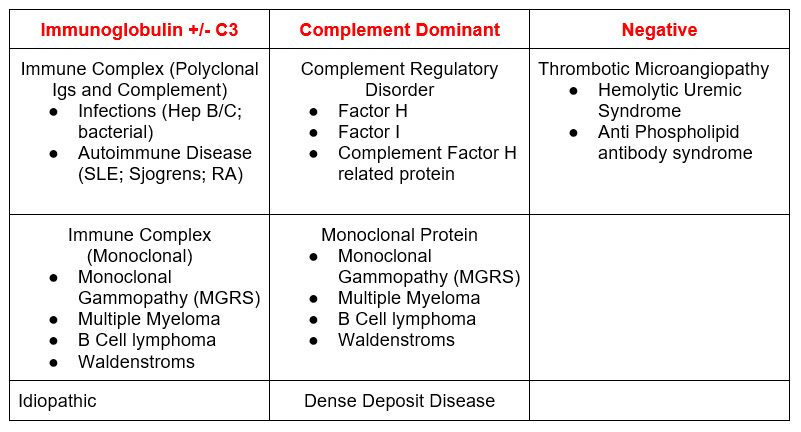
These can be deduced by the pattern on immunofluorescence. Immunofluorescence can show:
- Immunoglobulin (with or without complement)
- Complement Dominant
- Immunofluorescence Negative (There are also cases without immune complexes)
Etiologies
Immunofluorescence
Tip:
One of the most common causes of MPGN is Hepatitis C related cryoglobulinemia
Evaluation
Initial findings
That will lead to suspecting this diagnosis include:
- Abnormal kidney function which may be deteriorating acutely or subacutely
- Abnormal urinalysis with microscopic hematuria and/or proteinuria
- Overt proteinuria
- Signs and symptoms of systemic vasculitis (palpable purpura, arthralgias, mononeuritis)
Subsequent evaluation
- Serum complements which are often low (particularly C4)
- Hepatitis C, 1st antibody, confirm with PCR
- Cryoglobulin: You can send this, but it is difficult to process. There are many false negatives as the specimen needs to be kept warm (or the cryoglobulins will precipitate).
- Rheumatoid factor. Mixed cryoglobulinemia is an IgM antibody against an IgG. This is a rheumatoid factor. (A rheumatoid factor is an IgM antibody directed against the Fc portion of IgG)
- Serum immunoglobulins and free light chains. These may be elevated. As Type II cryoglobulinemia (the type associated with hepatitis C) contains a monoclonal IgG vs a polyclonal IgG, you may see a polyclonal elevation on serum immunofixation.
Kidney Biopsy
Necessary to confirm the diagnosis.
Treatment
The primary approach to treatment should be directed against the underlying pathophysiologic cause of MPGN.
- Hepatitis C – Direct acting antiviral
- Rheumatologic disease – Immunosuppression (ie. mycophenolate, rituximab, steroids)
- Monoclonal protein – Treatment against the monoclonal protein (ie. bortezomib)
Other treatment options are dependent on the clinical context
- Supportive care (Renin angiotensin system blockers)
- Proteinuria < 3.5 grams/ day; normal eGFR
- Advanced disease (eGFR < 30 without active inflammation on biopsy)
- Severe tubulointerstitial fibrosis on biopsy
- Glucocorticoids (Prednisone 1 mg/kg day for 12-16 weeks, followed by taper)
- Nephrotic syndrome, normal or near normal eGFR
- Immunosuppression (Cyclophosphamide, rituximab, mycophenolate) with steroids
- Abnormal kidney function with nephritic urinary sediment (glomerular hematuria +/- proteinuria)
- Rapidly progressive glomerulonephritis (RPGN). (Pulse followed by oral glucocorticoids + cyclophosphamide)
- C3 glomerulopathy (MMF + glucocorticoids)
- Eculizumab
- C3 glomerulopathy
Summary
Membranoproliferative Glomerulonephritis (MPGN) is a condition with a wide range of clinical presentations. The underlying pathophysiology can be deduced by kidney biopsy immunofluorescence. This guides secondary evaluation. Becoming expert at assessing the varying clinical presentations is critical in determining the best treatment options.



