Table of Contents
This article will address:
- Diagnosis of metabolic alkalosis and assessment of compensation.
- Approach to differential diagnosis/ underlying cause of metabolic alkalosis.
Metabolic Alkalosis Diagnosis
- Elevated pH (>7.42)
- Elevated serum HCO3– (>26)
- Elevated pCO2 (compensation)
What you will initially see (either in the hospital or outpatient setting) is an elevated serum HCO3. This can represent either a metabolic alkalosis or a respiratory acidosis. This scenario is not uncommonly seen in hospitalized patients with dyspnea who have CHF treated with diuretics and underlying COPD. These patients have reasons for both a metabolic acidosis (contraction alkalosis from diuresis) and respiratory acidosis (from COPD).
OK so you have an elevated HCO3 and pH. How do you know if the response is appropriate?
- Easiest way: Add 15 to the HCO3, that’s the expected pCO2
- Another way: Change in pCO2 = 0.7 Change in HCO3
Physiology Pearl:
Metabolic alkalosis can be thought of as having too much bicarbonate (HCO3–) in the body. Physiologically, the loss of a Hydrogen Ion (H+) is the same thing as retaining a Bicarbonate Anion (HCO3–).
The following biochemical reaction occurs in the body:
H+ + HCO3– ⇄ H2CO3 ⇄ H20 + CO2
Approach to Differential Diagnosis
The main approach to differential diagnosis is Chloride responsive/resistant. Another way to break it down is Elevated blood pressure vs. Normal/low blood pressure.
Chloride responsive
- Reflects volume contraction/depletion
- Usually extrarenal loss of HCl and NaCl
- Often associated with low or normal BP
- Urine Chloride < 25
Chloride resistant
- Usually (but not always) reflects volume expansion
- Caused by inappropriate renal excretion of HCl and NaCl or gain of exogenous alkali
- Usually (but not always) is associated with elevated BP
- Urine Chloride > 40
Why Urine Chloride?
Typically volume status (contraction vs expansion) can be assessed by the urine sodium. Volume contracted states will have a low urine sodium. However, this doesn’t work for metabolic alkalosis. Why not? If there is a metabolic alkalosis there may be bicarbonate excretion in the urine as an attempt to correct the alkalosis. (typically most if not all hco3 is reabsorbed in the proximal tubule). Remember HCO3 is an anion, it is negatively charged. When it’s excreted in the urine it has to bring something positively charged with it. This is either sodium or potassium. So the urine sodium will be high with metabolic alkalosis even if volume contracted. It is also why metabolic alkalosis is often associated with hypokalemia.
So the best urine test to assess for volume contraction in metabolic alkalosis, the urine chloride. The kidney can’t hang on to sodium, but it can hang on to chloride.
Differential Diagnosis: Chloride Responsive Metabolic Alkalosis
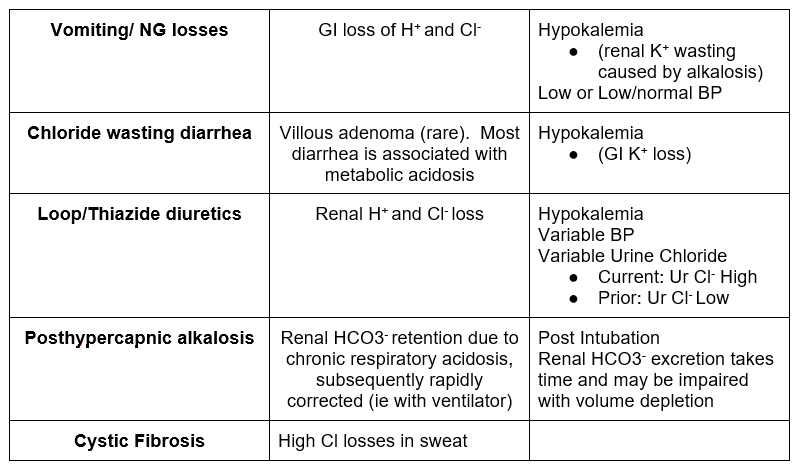
Differential Diagnosis: Chloride Resistant Metabolic Alkalosis
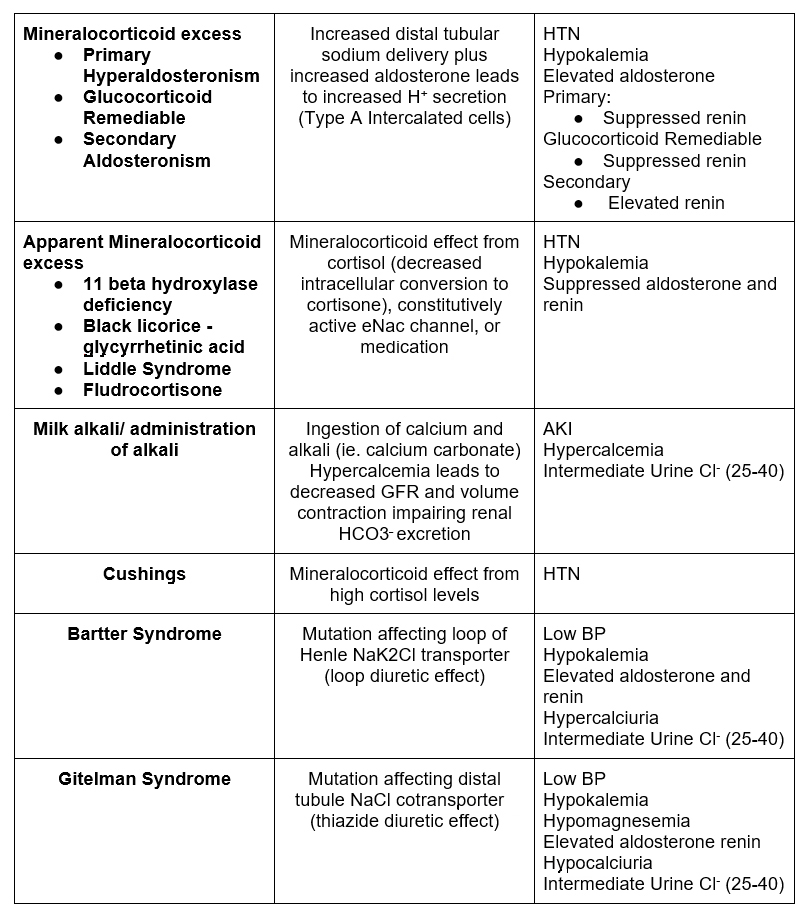
Differential Diagnosis: BP approach
Elevated BP
- Mineralocorticoid excess
- Primary Hyperaldosteronism
- Glucocorticoid Remediable Aldosteronism
- Secondary Aldosteronism
- Apparent mineralocorticoid excess
- 11 beta hydroxylase deficiency
- Black licorice – glycyrrhetinic acid
- Liddle Syndrome
- Fludrocortisone
Low/normal BP
- GI losses
- Vomiting
- NG loss
- Chloride rich diarrhea
- Bartter syndrome
- Gitelman syndrome
Variable BP:
- Diuretics
- Loop
- Thiazide
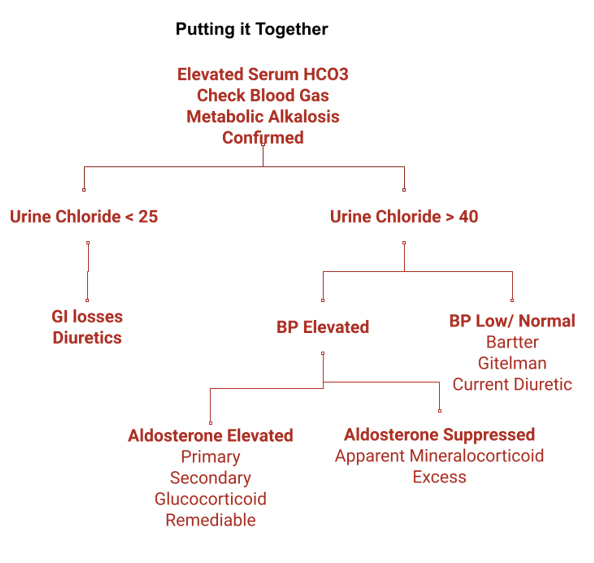
Summary – Steps in assessment
- Finding of elevated serum HCO3–
- Check blood gas to confirm metabolic alkalosis
- Serum calcium elevated – consider milk/calcium alkali syndrome
- Assess Urine Chloride
- < 25 – GI losses, diuretics, posthypercapnic; cystic fibrosis
- > 40 – Assess BP
- BP elevated
- Check aldosterone and renin
- Aldosterone High (Primary, Secondary, Glucocorticoid remediable aldosteronism
- Aldosterone Low (Apparent mineralocorticoid excess – Liddle, 11 beta hydroxylase deficiency/black licorice cushings)
- Check aldosterone and renin
- BP low / normal (Bartter; Gitelman)
- BP elevated



