Table of Contents
Membranous nephropathy is an important cause of nephrotic syndrome in adults.
This condition is exciting in nephrology because the pathogenic antibody for the majority of cases of primary idiopathic membranous nephropathy has been discovered. This is the phospholipase A2 receptor (PLA2R) antibody.
Clinical Presentation
- Often presents as full blown nephrotic syndrome with severe proteinuria with hypoalbuminemia and edema
- Can present with non nephrotic proteinuria.
- Often has a preserved glomerular filtration rate (GFR) at presentation.
- Can result in chronic kidney disease (CKD), if the proteinuria is chronically severe
- Rare cause of end stage kidney disease (ESRD).
- Not an acute or rapidly progressive glomerulonephritis, but can be associated with acute kidney injury (AKI) via the mechanism of renal vein thrombosis.
The chief complaint is often edema, patients may also report a foamy character to the urine. A patient with this presentation should have the following evaluation:
- CMP (for creatinine, eGFR, and albumin)
- Urinalysis with additional quantitation of proteinuria (random urine protein creatinine ratio).
In Membranous nephropathy this evaluation will reveal hypoalbuminemia and nephrotic proteinuria which may be severe. Once this is found a serologic evaluation for nephrotic proteinuria should be performed.
An important part of the serologic evaluation in adults with nephrotic syndrome is the phospholipase A2 receptor (PLA2R) antibody. This is positive in about 80% of cases of primary idiopathic membranous nephropathy and has a high specificity (99%).
If the PLA2R antibody is positive, even though this is diagnostic, strong consideration should be given to obtaining a kidney biopsy. I typically will perform a biopsy although an argument can be made not obtain one if:
- Immunosuppressive therapy is not planned
- There is an absolute or strong relative contraindication to renal biopsy.
Kidney biopsy in membranous nephropathy reveals:
- Light Microscopy: Glomeruli show thickening of the basement membrane. Silver stain has a characteristic spike pattern.
- Immunofluorescence: Granular IgG and C3
- Electron Microscopy: Subepithelial deposits (immune complexes) are characteristic. (Most other GN’s show either mesangial or subendothelial deposits)
The biopsy can also be stained for PLA2R antibody to confirm that the Membranous Nephropathy is Primary.

What to do once Membranous Nephropathy is Diagnosed
Okay, now we know its membranous nephropathy, what do we do now?
- Figure out if it’s primary or secondary.
- General management.
- Assess risk to decide on immunosuppression
Differentiate primary vs secondary
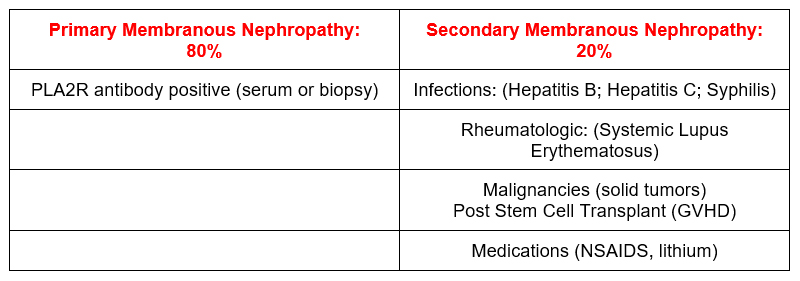
If the PLA2R antibody in the serum and immunostain on the kidney is negative, evaluation for the secondary causes should be performed. This includes.
- Hepatitis B surface antigen, Hepatitis C antibody, +/- RPR
- ANA, DSDNA, C3, C4
- Age appropriate cancer screening (breast, colon, prostate), +/- CXR
Age appropriate cancer screening should be done regardless of the PLA2R antibody status.
There is another pathogenic antibody that is associated with membranous nephropathy secondary to malignancy. This is the Thrombospondin type-1 domain containing 7A (THSD7A) antibody. An immunostain for this can be performed on kidney biopsy specimens that are negative for PLA2R.
General Management
All patients with membranous nephropathy should have the following general conservative treatment:
- RAAS blockers (for proteinuria)
- Loop diuretics (for edema)
- Blood pressure control
- Lipid assessment and treatment (statin)
- Assessment of Thrombotic Risk and need for prophylactic anticoagulation.
Membranous nephropathy may be the nephrotic syndrome most associated with venous thrombosis. This may be renal vein thrombosis (classically described with AKI, hematuria, and flank pain) or a pulmonary embolism.
The risk of thrombosis is directly related to serum albumin. I would strongly consider anticoagulation with warfarin or apixaban if albumin < 2.0, some would consider if albumin < 2.5. If albumin is more minimally decreased then consider aspirin.
There is a risk calculator to help you decide on prophylactic anticoagulation. Prophylactic Anticoagulation in Patients with Membranous Nephropathy: A Decision Analysis
Assess risk
There is a significant chance of spontaneous remission in membranous nephropathy. Therefore it is often appropriate to wait 6 months prior to initiating immunosuppression unless there is a high risk of progression. The risk of progression is determined by:
- Kidney Function
- Severity of Proteinuria and hypoalbuminemia
- PLA2R antibody titer
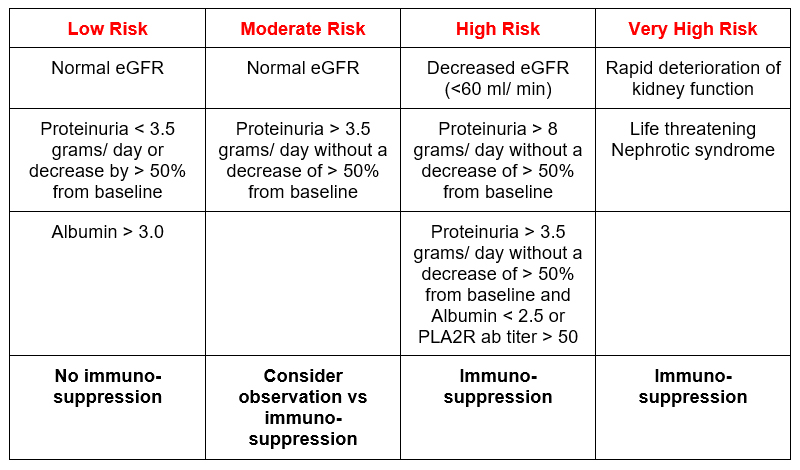
In primary membranous nephropathy a decrease in PLA2R antibody titers often precedes the decrease in proteinuria. This makes sense. First the body stops making the antibody then the antibody that is already deposited in the kidney needs to resorb and the glomerular basement membrane to heal.
Immunosuppression in Primary Membranous Nephropathy
Same options here as for most glomerular diseases except that corticosteroids are not used alone. Regimens are:
- Cyclophosphamide based:
- Calcineurin inhibitor based:
- Rituximab based:
Cyclophosphamide based
One of the original regimens was the Ponticelli regimen. This was chlorambucil alternating with steroids every other month for 6 months. Most nephrologists would not use chlorambucil. There is an alternate regimen of cyclophosphamide alternating with steroids every other month.
- Months 1,3,5: Pulse methylprednisolone x 3 days followed by daily oral prednisone (0.5 mg/ kg /day)
- Months 2,4,6: Oral cyclophosphamide (2.5 mg/kg/day) without steroids.
This regimen of alternating every other month seems odd to me. I prefer to use a concomitant regimen of steroids and lower dose cyclophosphamide for 6 months.
- Months 1,3,5: Pulse methylprednisolone x 3 days
- Oral prednisone (0.5 mg/ kg /day)
- Oral cyclophosphamide (1.5 mg/kg/day) without steroids.
I have had good success with this regimen in inducing remission without relapse. Remember to monitor CBC with diff twice a month, and decrease the dose of cyclophosphamide if there is leukopenia.
Calcineurin inhibitor based
- Cyclosporine 3.5 mg/kg/day (divided in two daily q 12 hour doses) with a target trough of 125-225.
- Tacrolimus 0.05-0.1 mg/kg/day (divided in two daily q 12 hour doses) with a target trough of 3-8
- I often add low dose prednisone (ie. 10 mg every other day).
Remember these drugs are associated with a higher risk of relapse after discontinuation. They also can be nephrotoxic. They are most appropriate for patients with a preserved GFR and more modest proteinuria (< 8 grams/day)
Rituximab based
This regimen is 1 gram dosed twice separated by 2 weeks. It has become popular since the discovery of the pathologic PLA2R antibody
Summary
Membranous Nephropathy presents as nephrotic syndrome with or without preserved GFR. The chief complaint is edema. Evaluation shows hypoalbuminemia and nephrotic range proteinuria. It may be associated with venous thromboembolism (renal vein thrombosis or pulmonary embolism). There are primary and secondary forms. The Phospholipase A2 receptor (PLA2R) antibody has become important in distinguishing primary vs secondary and monitoring for evidence of remission.
For more information check out chapter 3 of the Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guideline.



