Table of Contents
Many, if not most patients with chronic kidney disease (CKD) will have indications and benefit from pharmacologic treatment of hyperlipidemia. Despite this patients and some clinicians may have concerns about nephrotoxicity with use of these medications.
This article will review the data regarding renal safety and the potential for adverse renal effects of common medications used in the treatment of hyperlipidemia.
Statins
The most common lipid lowering agents are statins. These medications are HMG-CoA (3-hydroxy-3-methylglutaryl coenzyme A) reductase inhibitors. This enzyme is involved in cholesterol biosynthesis.
What does the data say about?
- Acute Kidney Kidney Injury
- Rhabdomyolysis
Acute Kidney Injury
Can statins cause acute kidney injury (AKI)? Let’s look at the data.
This study retrospectively looked at the incidence of acute kidney injury (AKI) with high and low potency statins.
It found an increased risk of hospitalization for AKI in 120 days of high dose vs low dose statin initiation
- No baseline CKD: 34%
- 1700 needed to treat for 1 AKI hospitalization
- Baseline CKD: No statistically increased risk of AKI hospitalization.
However, a subsequent metaanalysis did not find an increased incidence of AKI with statin.
- Results of trials totaling 149,882 patient years did not show any increase in serious adverse events in statins compared to controls.
Bottom line: The risk of AKI from statins is exceedingly low.
Rhabdomyolysis
Although muscle symptoms with statins may be common, rhabdomyolysis is rare with statins currently in use.
- Clinical significant myonecrosis, defined as a creatine kinase (CK) elevation > 10 times the upper limit of normal occurs in < 0.5% of patients.
- There was one statin cerivastatin (BayCol) that had a significantly higher rate of rhabdomyolysis. This was taken off the market in 2001.
- Hospitalization for rhabdomyolysis is even rarer
This study examined the incidence of hospitalization for rhabdomyolysis with:
- Statins (atorvastatin, pravastatin, simvastatin)
- Fibrates (gemfibrozil, fenofibrate)
- Combination statins and fibrates
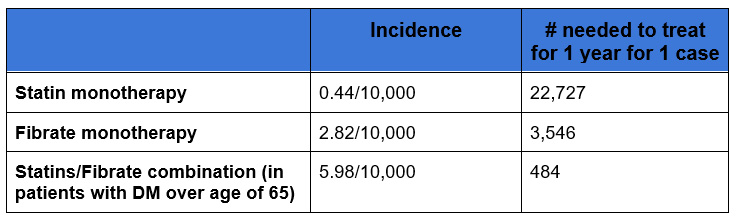
Conclusion: The risk of rhabdomyolysis with current statins is low. The risk increases when used in combination with fibrates.
YouTube: Do I Have Rhabdo @BCNephro
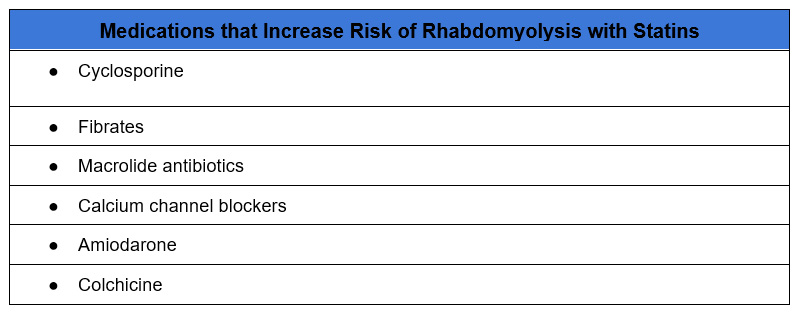
The risk of rhabdomyolysis with statins increases with the following:
- Higher dose statin
- Statins metabolized by cytochrome p450 3A4 (CYP3A4) – lovastatin, simvastatin atorvastatin
- Hypothyroidism
- Vitamin D deficiency
- Concurrent medications that either inhibit CYP3A4 or have independent risk of muscle toxicity
Fibrates
Fibrates work by activating peroxisome proliferator activated receptors (PPARs). They are most commonly used to treat hypertriglyceridemia.
The most commonly used fibrates are:
- Fenofibrate
- Gemfibrozil
Both have an association with rhabdomyolysis, particularly when used in combination with statins.
In addition, fenofibrate can have an adverse effect on kidney function.
Fenofibrate Nephrotoxicity
Fenofibrate often causes a reversible increase in kidney function. I observe this often clinically. When I am referred a patient for abnormal kidney function one of the things I look for is if they are on fenofibrate. If they are, I look to decrease the dose or discontinue fenofibrate. With this the kidney function often improves. Gemfibrizol doesn’t seem to have this effect.
How does fenofibrate affect kidney function? There are several proposed potential mechanisms
- Decreased tubular secretion of creatinine
- Increased creatinine generation from muscles
- Hemodynamic effects on glomerular circulation (afferent arteriole) mediated by decreased prostaglandins.
This study examined the effects of fenofibrates on renal function.
This study looked at patients in the ACCORD study treated with fibrates. In this study a group was treated with fenofibrate at a dose of 160 mg
- Dose decreased to 54 mg if eGFR < 50 on 2 consecutive occasions
- Discontinued if eGFR < 30 on 2 consecutive occasions
It looked at patients after the study close out (mean 5 yrs) who had:
- Creatinine increase of > 20% after fibrate initiation (47.4%). This happened within 3 months of initiation.
And compared them to patients who had:
- Creatinine increase of < 2% after fibrate initiation (controls) (24.6%)
- Patients treated with placebo.
It found:
- Creatinine improved after 51 days of discontinuation of fenofibrate.
- To levels not different from placebo
- Remained higher than controls.
- Changes in cystatin C were similar to those in creatinine
Conclusions:
- That cystatin C changes were commensurate with those of creatinine suggests that impaired tubular secretion or increased muscle generation of creatinine.
- That the changes were reversible after several years suggests that the decrease in GFR is based on glomerular hemodynamics (i.e. a decrease in vasodilatory prostaglandins).
- That the control group (those with < 2% initial creatinine increase with fenofibrate) continued to have a lower creatinine suggest that fenofibrate may have a renoprotective effect in a subset of patients.
- There may be a subset of patients with a more significant effect of fenofibrate on kidney function given the study protocol of discontinuation with an eGFR < 30 on two occasions.
Creatinine Cystatin C and GFR @BCNephro
Creatinine, Cystatin C and GFR
Ezetimibe
Ezetimibe works by impairing intestinal absorption of cholesterol.
Although there are case reports, rhabdomyolysis is exceedingly rare with ezetimibe.
There is no other evidence of nephrotoxicity and some evidence to suggest renoprotection.
Renal and Vascular Protective Effects of Ezetimibe in Chronic Kidney Disease
PCSK9 inhibitors
PCSK9 is a protein that degrades LDL receptors on the liver. PCSK9 inhibitors lower LDL by impairing this degradation.
- Evolucumab (Repatha)
- Arilocumab (Praluent)
- Inclisiran (Leqvio)
These medications are considered safe for the kidneys and there is some evidence of renoprotection.
Bempedoic acid
Bempedoic acid (Nexletol) inhibits adenosine triphosphate citrate lyase. This is an enzyme upstream of HMG-CoA. It is less potent than statins, but not associated with muscle symptoms.
Bempedoic acid may have an effect on renal function, however this is typically small and not clinically meaningful. Although data is limited there is no evidence of significant nephrotoxicity.
Evaluating the effect of bempedoic acid on kidney function: call for cautious implementation – Authors’ reply – The Lancet Diabetes & Endocrinology.
Summary
Statins and fibrates have a risk of rhabdomyolyis, particularly when used in combination. However, this risk remains relatively low. In addition, fenofibrate is often associated with a reversible worsening in serum creatinine and GFR. Aside from this there is no convincing evidence of significant nephrotoxicity from lipid lowering medications.



