Table of Contents
Infection associated glomerulonephritis. Patient presents with Acute Kidney Injury (AKI) and active urine sediment in the context of a current or recent infection.
Pathophysiology and Clinical Presentation
Antigen antibody immune complexes form with the antigen from the infection and the antibody from the immune response. These immune complexes deposit in the glomeruli inducing an inflammatory response involving complement.
The result: An endocapillary proliferative glomerulonephritis.
This presents clinically with:
- AKI
- Active urine sediment (hematuria, proteinuria, leukocyturia)
- Low C3
Renal Biopsy
- Light Microscopy
- Most Common:
- Diffuse endocapillary proliferative and exudative glomerulonephritis
- Less Common:
- Focal proliferative / mesangial proliferative glomerulonephritis
- Necrotizing crescentic glomerulonephritis
- Membranoproliferative glomerulonephritis
- Immunofluorescence
- Starry Sky Pattern
- C3 with IgG
- C3 with IgA (Staphylococcal variant)
- C3 alone
- Electron Microscopy
- Subepithelial humps
- Other deposits may be present (mesangial, subendothelial, intramembranous)
- Most Common:
Classic Infectious GN
Classic infectious GN was described in the following circumstances:
- Post streptococcal (PSGN). Certain strains of group A beta – hemolytic streptococcus have a “nephritogenic antigen”, resulting in an immune complex mediated endocapillary proliferative GN.
- Typically occurs in children
- Presents with hematuria @ 1-2 weeks after the infection (typically pharyngitis)
- Good prognosis
- Positive streptozyme (streptococcal antibody) in 80-95%
- Antistreptolysin (ASO)
- Anti-hyaluronidase
- Anti-streptokinase
- Anti-NAD
- Anti-DNase B
- Endocarditis
- Persistent bacteremia allows for systemic immune complex formation
- Shunt nephritis
- Infected ventriculoatrial (VA) shunts can result in persistent bacteremia as in endocarditis
- Less common as most
In my experience I have not encountered these presentations often.
- PSGN typically occurs in the pediatric population
- PSGN may be less common with the advent of rapid testing and more common use of antibiotics.
- Although endocarditis does occur, most shunts currently are ventriculoperitoneal (VP) shunts. Although these can become infected they typically are not associated with bacteremia.
Modern Infectious GN
A new variant of infectious GN mimicking IgA nephropathy was described in 2006.
Staphylococcus Infection-Associated Glomerulonephritis Mimicking IgA Nephropathy
This variant of infectious GN presents in older patients with diabetes and staphylococcal infections (often without bacteremia – such as diabetic foot infections or osteomyelitis).
IgA nephropathy was always in the differential of infectious GN as both conditions present clinically as hematuria in the context of infection. However, renal biopsy immunofluorescence would distinguish showing IgG in infectious GN and IgA in IgA nephropathy.
However, the staphylococcal form of infectious GN is associated with IgA deposition on renal biopsy.
Staph associated GN characteristics
- Risk factors: Increased age, diabetes mellitus, cancer
- Occurs concomitantly with infection (as opposed to post infectious)
- Types of infections: Endocarditis, empyema, osteomyelitis, skin, indwelling catheter, shunt
- May have vasculitic skin rash
- Urinalysis
- Hematuria 98% (15% macroscopic)
- Leukocyturia 65%
- Proteinuria (21% nephrotic syndrome)
- Low C3: 80%
- ANCA positive: 22%
- Renal biopsy immunofluorescence: IgA dominant or codominant
Differential Diagnosis
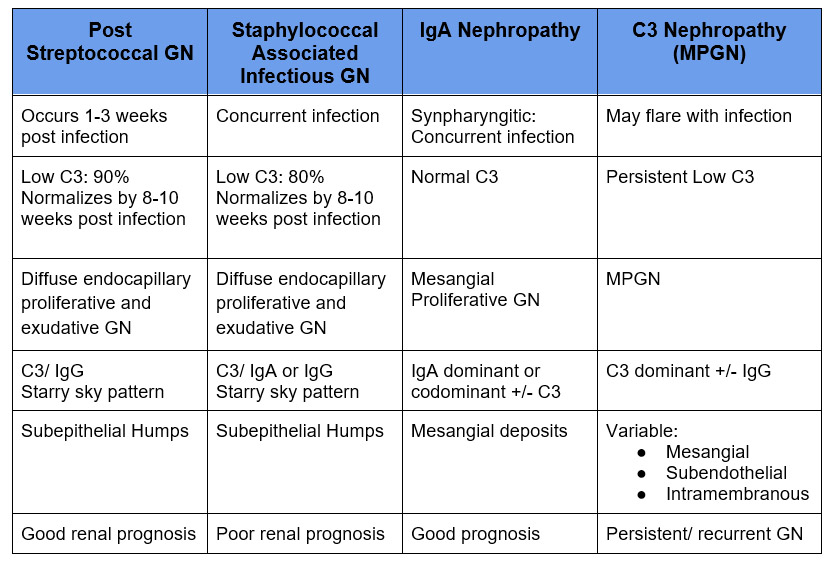
Infection related GN shares clinical findings with IgA nephropathy and C3 Nephropathy (variant of MPGN). Infection associated GN is caused by the infection, but both IgA nephropathy and C3 Nephropathy can flare with AKI and hematuria during an infection.
Treatment
Treatment is supportive. Patients with baseline diabetic kidney disease have a poor renal prognosis.
No underlying diabetic nephropathy:
- 56% complete remission
- 27% persistent kidney disease
- 17% progressed to End stage kidney disease (ESRD)
Underlying Diabetic nephropathy:
- 18% persistent kidney disease
- 82% progressed to ESRD
Steroids are not effective and are associated with an increased incidence of adverse effects.
- Complete recovery: 65% vs 55% (not significant)
- Increased adverse effects: 46% vs 8%
Summary
Glomerulonephritis may present in the context of infections. The GN may be infection associated or a sign of underlying IgA nephropathy or C3 nephropathy. Clinical and biopsy findings may overlap making astute clinical judgment and close follow up necessary.



