Table of Contents
You know or can look up the standard diagnostic algorithm for hyponatremia.
- Hypovolemic
- Euvolemic
- Hypervolemic
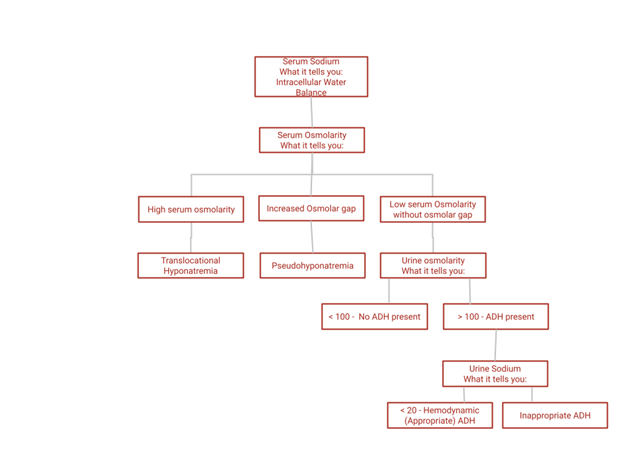
Not doing this here. Read on to find out what the labs tell you. Knowing this will supplement and deepen your understanding. We’ll be analyzing the following labs:
- Serum Sodium
- Serum Osmolarity
- Urine Osmolarity
- Urine Sodium
- Uric acid
Serum sodium: What it tells you
Hint: If your answer has sodium in it you’re wrong.
You already know this. The standard algorithm is hypovolemic (too little sodium), euvolemic (normal sodium), hypervolemic (too much sodium). If that doesn’t click, think of this. What do you do for a hypovolemic patient? You give saline. What do you do for a hypervolemic patient? You put them on a sodium restriction.
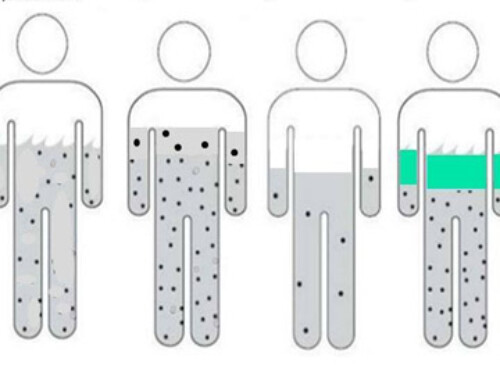
Since water goes down the osmotic gradient (intracellular to extracellular or vice versa) in hypotonic hyponatremia water goes from the extracellular to intracellular space.
You already know this too. What are the symptoms of severe hyponatremia? CNS side effects, caused by swelling of brain cells.
The serum sodium doesn’t tell us the sodium balance of the patient. The sodium balance is the (extracellular) volume status of the patient. We know a hyponatremic patient can be hypovolemic (low total body sodium), euvolemic (normal total body sodium) or hypervolemic (elevated total body sodium).
The serum sodium tells you the intracellular water status.
Serum osmolarity: What it tells you
If you answer is “If the patient is hypotonic or hypotonic”, well yes the answer is right, but we’re going deeper here. What does that mean? What’s the physiology?
First things first we want to rule out pseudohyponatremia. Pseudohyponatremia is a lab artifact. Here’s what happens:
- Normal serum is 93% liquid and 7% solid (i.e. proteins).
- When the lab runs a chemistry panel the serum is diluted.
- The reported result is calculated from the measured result based on this 93% liquid, 7% solid assumption.
- There are conditions, such as severe hypertriglyceridemia, where the % solid phase is higher.
- Example: The patient has a disease state where the serum is 86% liquid and 14% solid, the lab uses the 93% conversion factor and reports a falsely low number.
This is pseudohyponatremia.
You figure this out by calculating the osmolar gap. In pseudohyponatremia the measured serum osmolarity will be significantly higher than the calculated (2 x Na + glucose/18 + BUN/2.8) osmolality.
If you’re really interested read this:
Mind the Gap | New England Journal of Medicine
Another way to diagnose this is to check the sodium on a blood gas specimen. Blood gas samples are not diluted prior to analysis so are not subject to pseudohyponatremia.
The serum osmolarity lets you calculate the osmolar gap which tells you if the hyponatremia is real
What else can the serum osmolarity tell you?
If the serum osmolarity is high as in severe hyperglycemia…
This is NOT pseudohyponatremia, it is translocational hyponatremia. The sodium is really low. The reason it’s low is hyperglycemia provides an osmotic gradient to pull water out of cells and dilute the sodium down. It’s not a lab artifact.
Urine osmolarity: What it tells you
Question. If you are hyponatremic (assuming you are normal), how dilute should your urine be?
Answer. As dilute as it can.
Think about it. If you drink a gallon of water what happens? You pee a gallon of water. Not over a couple of days or a week, as fast as your body can do it.
So how dilute can urine be? The range of urine osmolarity is 50-1200, by convention a urine osmolarity of < 100 is considered maximally dilute.
So:
Urine osmolarity < 100 – no ADH present
Urine osmolarity > 100 – ADH present
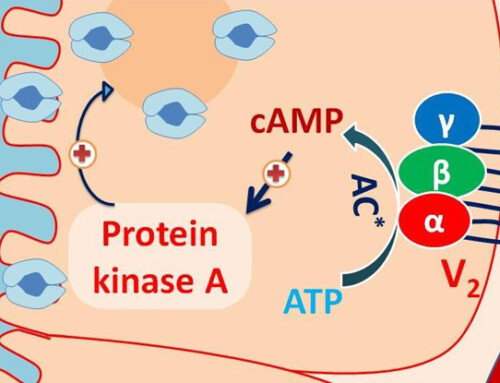
(There is one exception you probably don’t need to know, but I’m a nephrologist so I do know. NSIAD – Nephrogenic syndrome of Inappropriate Antidiuresis. This means there is a bum vasopressin (ADH receptor) that is constitutively turned on.
Your differential for hyponatremia if urine osmolarity is < 100 (No ADH present)
- Primary polydipsia
- Poor solute intake. “Tea and toast diet” or “beer potomania”. The observation for beer potomania is the urine osmolarity is typically between 100-200, that’s just what is.
The urine osmolarity tells you if ADH is present.
Urine sodium: What it tells you
OK, if ADH is present we want to figure out why? Is it appropriate or inappropriate?
Reasons for ADH to be present
- Osmotic (appropriate). This is the main reason. If you’re really dehydrated your serum sodium goes up, your serum osmolarity goes up and your body hangs on to water by producing ADH, resulting in concentrated urine. But, we’re working up hyponatremia now, so this is not the case.
- Non – Osmotic
- Hemodynamic (appropriate). If you’re in shock the body doesn’t say “Wait a minute the sodium is low we better pee out all that water so the sodium goes back to normal.” if you’re in shock the body holds on to all the water it can so you don’t die.
- SIADH (inappropriate).
If the body is in such a bad hemodynamic state that it’s hanging on to water, what else is it hanging on to?
It’s hanging on to sodium. The urine sodium is typically < 20 in these cases.
The urine sodium tells you if there is a hemodynamic (appropriate) reason for ADH to be present.
Your differential for hyponatremia if the urine osmolarity is > 100 and urine sodium < 20.
- True hypovolemia
- Decreased effective arterial volume (3rd spacing) – heart failure, cirrhosis
If the urine osmolarity is > 100 and urine sodium is high (> 40 typically in algorithms) your thinking SIADH < 20..
Uric acid: What’s the deal?
Patients with SIADH may not actually be “euvolemic”, they may be subclinically hypervolemic. This dilutes down the uric acid. So a uric acid < 4 suggests
SIADH. Not definitive, but can be a supporting clue.
Summary
- The serum sodium tells us the intracellular water balance
- The serum osmolarity lets us figure out if there is pseudohyponatremia or translocational hyponatremia
- The urine osmolarity tells us if there is ADH present
- The urine sodium tells us if the ADH is hemodynamic and therefore appropriate
- The uric acid can give evidence to support the diagnosis of SIADH