Table of Contents
As a nephrologist I get sent patients with resistant or difficult to control HTN. Here’s an approach, why I do it and what it tells me.
24 hour ambulatory BP monitoring
What it tells me: Is it really HTN or is it pseudo resistance?
- White coat syndrome, white coat effect
- Technique of measurement.
The machine used in the Sprint trial automatically took the BP 3 times separated by a minute, without a doctor or nurse in the room and averaged these 3 readings. SBP on average is about 5 points lower than traditional office measurement. I tell patients to do home BP in a similar manner. Sit for 5 minutes with arm supported on table, take 3 readings separated by a minute and average 2nd/3rd reading
- Other causes of pseudo resistance: Medication adherence, other medications (NSAIDS)
Renal Evaluation
Metabolic panel and Urinalysis
What it tells me: Is there kidney disease?
- The most common cause of secondary hypertension is probably kidney disease.
Renal Ultrasound
What it tells me: Is there structural kidney disease?
- Everyone sent to me for resistant hypertension gets a renal ultrasound (not necessarily with dopplers of renal arteries, plain renal ultrasound).
- Looking for structural kidney disease (like polycystic kidney disease); significant asymmetry in kidney sizes which may be a clue to renal artery stenosis.
My opinion: Renal artery stenosis screening is done too frequently. Many patients with RAs can be treated medically. If the patient has chronic HTN and especially if they also have CKD they will still have HTN even after a renal artery stenosis is revascularized.
Screening for RAS is most appropriate if the HTN is of relatively new onset (such as FMD in a young woman or new HTN with renal artery stenosis, +/- abdominal bruit in an older patient).
There are many false positive and false negative renal artery doppler studies. If there is high clinical suspicion (or confirmation required) a CTA or MRA of the renal arteries should be performed
Aldosterone Renin Ratio
What it tells me: Screen for Primary Hyperaldosteronism
- Primary hyperaldosteronism. Thinking about this if hypokalemia, but an aldosterone renin ratio is always part of my evaluation for resistant HTN as a nephrologist. The aldosterone needs to be high (above 20) with a high ratio (above 20) for this to be the case. Be careful of a high ratio with a very low renin, a denominator < 1 can make the ratio very high.
- Helpful even if the screen is not positive for hyperaldosteronism. A very low renin (< 0.6), suggests volume or sodium mediated HTN. In this case addition or intensification of the diuretic regimen is appropriate. If low renin in a patient with RAS, I would be less optimistic that renal artery revascularization will be helpful.
Plasma Free Metanephrines
What it tells me: Screen for Pheochromocytoma
- Not very common. Plasma metanephrines are my screen here. Thing to remember is that in pheo these are REALLY high, more than 4 times upper limit of normal. If mildly elevated more likely due to stress or other medications.
Medications
What it tells me: Do the medications make sense?
- It’s not resistant if the patient is not on an appropriate diuretic. Most commonly a thiazide, but some may need a more potent diuretic, especially if CKD. Traditionally had been taught that thiazides are not effective in advanced CKD (stage 4 or higher), but this article suggests otherwise:
https://www.nejm.org/doi/full/10.1056/NEJMoa2110730
I typically have not used loop and thiazide type diuretics together (with the exception
of metolazone in refractory edematous states), but the combination was used in this study. A subset of patients were treated with torsemide 10-20 mg per day. When appropriate I’m going to try the combination using either torsemide or chlorthalidone with the other three days a week.
- RAAS blocker (ACE-I or ARB). Remember RAAS blockers are synergistic with thiazides and calcium channel blockers, but not beta blockers.
- Avoid medications that are difficult (and therefore less likely) for the patients to take. Talking about tid meds and meds that make the patient feel like crap. Clonidine, labetalol, and hydralazine are examples.
What it tells me: Are there other medications causing HTN
- NSAIDS
- Angiogenesis inhibitors
- Tyrosine Kinase inhibitors
- Decongestants
- Stimulants
- Atypical antipsychotics
To name a few
Summary
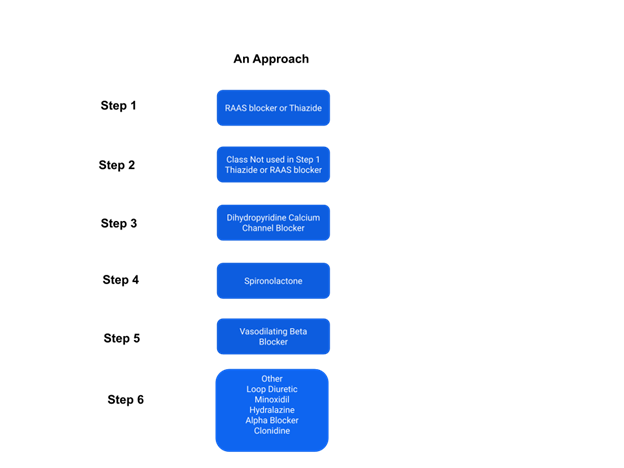
What tricks as a nephrologist do I have up my sleeve?
- Change Hydrochlorothiazide to Chlorthalidone. Chlorthalidone is more potent and has a longer half life. 25 mg chlorthalidone works better than 25 mg HCTZ
- Change furosemide to torsemide. Furosemide has a short half life (Lasix Lasts Six hours). To be used for HTN it should be given tid. Torsemide has a longer half life.
- Add spironolactone. The addition of spironolactone is often very effective in refractory HTN.
- Use dihydropyridine CCB. More effective than non-dihydropyridine (diltiazem/ verapamil). Also in my experience extended release nifedipine is more potent than amlodipine.
- Remember beta blockers are 5th line agents for HTN. RAAS blockers, thiazides, and CCB are top 3 (any order). Spironolactone should be 4th. If a beta blocker can try changing to a vasodilating beta blocker (ie carvedilol or nebivolol). I stay away from labetalol as I don’t think it is well tolerated.