Table of Contents
Hypernatremia like hyponatremia is all about water.
Hyponatremia indicates intracellular water excess (overhydration).
Hypernatremia means the opposite, too little water. (At least too little water relative to sodium). This is dehydration. It indicates intracellular dehydration.
This article will address:
- Pathophysiology
- Approach to Diagnosis
- Renal Causes of Hypernatremia
- Diagnostic Algorithm
- Treatment
Pathophysiology
What happens with hypernatremia is this:
- The serum osmolarity goes up. The serum sodium is the main contributor to the serum osmolarity (serum osmolarity = serum sodium x 2 + glucose/18 + BUN/2.8).
- Water leaves the cells via the osmotic gradient.
- The cells shrink.
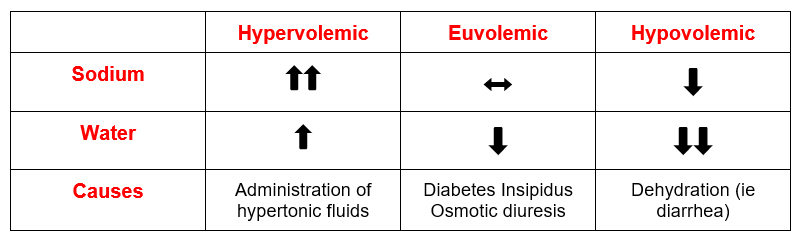
Hypernatremia can be:
- Hypervolemic: Increased total body sodium
- Euvolemic: Normal total body sodium
- Hypovolemic: Decreased total body sodium
In all cases there is too little water relative to sodium
Approach to Diagnosis
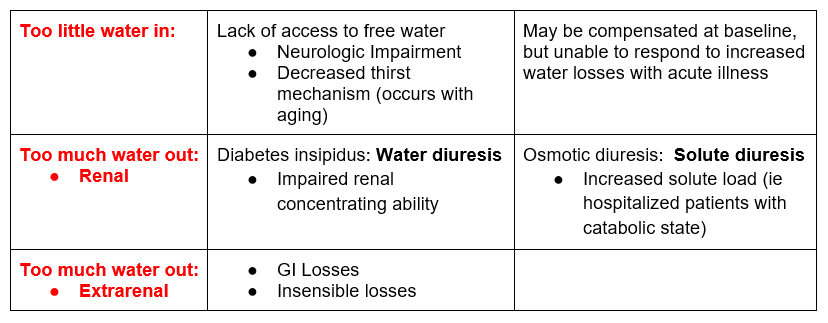
When approaching the diagnosis of hypernatremia (or electrolyte disorders in general) a useful approach is this.
- Is there too little (water) in?
- Is there too much (water) out?
- Renal water losses
- Extrarenal water losses
In all cases there is not enough water in to meet the water losses. The water losses may be normal insensible/metabolic losses or increased due to another pathological state.
Renal Causes of Hypernatremia
These are associated with polyuria (urine output > 3 liters/day)
Diabetes insipidus:
- Problem with ADH.
- Lack of ADH production (central diabetes insipidus)
- Resistance to ADH effect (nephrogenic diabetes insipidus). In my experience, nephrogenic diabetes insipidus due to current or prior lithium use is the more common etiology.
- Inability to concentrate the urine ➜ dilute urine ➜ polyuria from a water diuresis
- Low urine osmolarity typically less than 150.
By the way these patients are typically compensated as outpatients because they get thirsty and drink a lot of water. It’s when they get ill and can’t get or drink water that problems ensue.
Osmotic diuresis. What’s that?
- The kidneys have to excrete the daily osmolar load (sodium and protein metabolites). Essentially what comes in (in terms of salt and protein in the diet) must go out (in the urine as sodium and urea).
- Typical daily osmolar load that needs to be excreted in the urine is 600- 900 mOsm.
- Increased generation of osmoles may occur (such as in critically ill patients who have increased urea production from a catabolic state, treatment with corticosteroids and TPN as well as glucosuria from hyperglycemia).
- The increased osmolar excretion obligates urinary water excretion. (We don’t pee urea powder or sugar crystals)
- Urine osmolarity is typically > 300 mOsm/Liter. (Urine osmolarity > 300 mOsm/liter with urine volume > 3 liters a day = solute load > 900mOsm
Diagnoses: Putting it Together
- History: The history will often provide evidence of increased water losses and decreased access to water. Hypovolemic hypernatremia (dehydration).
- Urinalysis: Specific gravity. An elevated specific gravity on UA indicates the urine is concentrated which is an appropriate response to a water deficit (dehydration).
- Urine Output: Does the patient have polyuria? Polyuria is > 3 liters urine per 24 hours
- Diabetes Insipidus
- Osmotic Diuresis
Urine Osmolarity:
- Polyuria and urine osmolarity < 150 – consistent with diabetes insipidus.
- Polyuria and urine osmolarity > 300 – consistent with osmotic diuresis.
- No polyuria and high urine osmolarity – appropriate renal response to
Treatment
The treatment for a water deficit is to give water. Either oral, enteral feeding tube, or intravenously. The following questions are useful in treatment.
How much water to give?
The free water deficit can be calculated by the formula:
TBW x (serum Na/140 – 1)
Typically it is recommended to replace ½ the free water deficit in the first 24 hours.
What is the rate of correction?
Hypernatremia can safely be corrected (at least in adults) at a faster rate than chronic hyponatremia.
In hyponatremia the CNS cells are overhydrated (swollen) and lose idiogenic osmoles. When the hyponatremia is corrected rapidly the cells shrink which can result in central pontine myelinolysis. The recommended rate of correction is no more than 6-8 meq/L in the initial 24 hrs.
In hypernatremia the CNS cells are dehydrated (shrunken). When corrected the cells expand which can result in seizure. However, it is safe to correct by 12 meq/L (link)
https://journals.lww.com/cjasn/pages/articleviewer.aspx?year=2019&issue=05000&article=00006&type=Fulltext or more in the initial 24 hrs.
My patient is volume overloaded. I don’t want to give IV fluids.
Remember we are talking about intracellular dehydration. The majority of the free water you give will go into cells. If the water is in cells it’s not in the intravascular or interstitial space, it’s not causing pulmonary edema.
If the patient is hypernatremic and volume overloaded give free water and a loop diuretic. The concentration of urine induced by a loop diuretic is said to be equivalent to ½ NS. Therefore, if you diurese a patient 1 liter and give 1 liter of D5W they will have a net negative sodium balance (helping pulmonary edema) and positive water balance (500 ml) helping the hypernatremia.
Why is the hypernatremia not correcting?
Something that is commonly seen in the hospital setting: A patient is hypernatremic and is given free water, but the sodium is not coming down, or not coming down very much. What’s going on here?
The simple answer is you’re not giving enough water. I’m going to show you why.
You’ve calculated the free water deficit, administer the calculated amount of free water and nothing (or very little happens). What gives? Here are 2 possibilities.
- You’re giving potassium. Potassium counts. The deal is this. Most sodium in the body is extracellular, most potassium is intracellular. When you administer potassium, it goes into the cells exchanging for sodium. Giving potassium chloride has the same effect on serum sodium as giving sodium chloride.
If the IVF is ½ NS + 40 meq KCL per liter is effectively ¾ NS.
Bottom line: You’re not giving as much water as you think you are.
- You’re not counting ongoing water losses. These may be:
- Extrarenal water losses: Insensible water losses (which are increased with fever/ ventilator) and/or GI water losses.
- Urinary free water losses. There may be from a partial osmotic diuresis with urinary free water losses from hyperglycemia or urea (as occurs with recovery of prerenal acute kidney injury (AKI)).
Urinary free water losses can be calculated by the electrolyte free water clearance.
(1- Urine sodium + urine potassium) x urine volume.
Serum Sodium
Example:
Urine sodium 50
Urine potassium 25
Serum sodium 150
(1 – 50 + 25) = (1- 75) = (1-0.5) = (0.5).
150 150
What does this mean? It means for every liter of urine the patient is urinating 500 cc of free water. This will need to be added to the free water deficit when calculating the amount of free water to provide.
I don’t want to give D5 (My patient has hyperglycemia or an acute neurologic condition)
Often there may be a reluctance to give D5W because of hyperglycemia.
A useful way to think about fluids:
- Think of ½ NS as this. Half saline and half water.
- ½ NS 100 ml/hr is equivalent to separate infusions of NS 50 ml/hr and D5W 50 ml/hr
- If you intended to give D5W 100 ml/hr, but you can’t, then give ½ NS 200 ml/hr to provide the same amount of water.
Summary
Hypernatremia indicates a water deficit (at least relative to sodium). It results from a lack of sufficient water intake to meet water losses. Polyuria suggests renal losses of water. The urine osmolarity helps distinguish a water diuresis (diabetes insipidus) from an osmotic diuresis (increased solute load). There is more leeway to safely correct the sodium in hypernatremia than hyponatremia. Failure correction of hypernatremia suggests unaccounted for ongoing free water losses which may be urinary.
