Hypercalcemia is of interest to both nephrologists and endocrinologists.
Why nephrology?
- Hypercalcemia may cause acute kidney injury (AKI)
- Hypercalcemia, in specific primary hyperparathyroidism, is associated with nephrolithiasis (kidney stones).
- Secondary and Tertiary hyperparathyroidism is a complication of chronic kidney disease (CKD) and end stage renal disease (ESRD) primarily managed by nephrologists.
Bottom line: Hypercalcemia is an interesting condition and by approaching it with interest more cases will gravitate toward you.
Symptoms
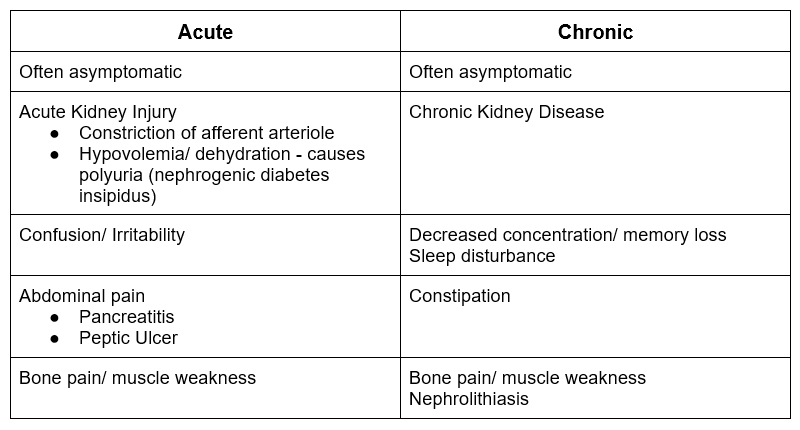
Hypercalcemia may be acute or chronic.
Moans, Bones, Stones and Groans
- Moans – Psychiatric symptoms: depression, anxiety, or irritability
- Bones – Musculoskeletal pain
- Stones – Nephrolithiasis
- Groans – Abdominal pain
Diagnostic Algorithm
Is it true hypercalcemia?
Look at the albumin. If the albumin is high or high/normal the true ionized calcium may be normal.
- Calculate corrected calcium
Corrected calcium = serum calcium + 0.8 x (patient’s albumin – normal albumin)
- Check ionized calcium
- Severe volume depletion/dehydration may also be associated with an elevated total calcium.
Are there medications associated with hypercalcemia?
The common ones are:
- Thiazide diuretics. These can cause hypercalcemia on their own or unmask subclinical primary hyperparathyroidism.
- Lithium. A cause of hyperparathyroidism
- Vitamin A or D toxicity. In a patient with CKD or ESRD look for treatment with active vitamin D (calcitriol).
Is the hypercalcemia mediated by parathyroid hormone (PTH)?
The main initial diagnostic decision point is whether the hypercalcemia is mediated by PTH or not.
- If the calcium is high, the PTH should be suppressed. A “normal” PTH is not normal if there is hypercalcemia. PTH should be < 25.
- If PTH is elevated or not suppressed – consider primary hyperparathyroidism
- If PTH is suppressed – continue evaluation for other causes of hypercalcemia.
Is there malignancy?
Malignancy is the most common cause of non PTH mediated hypercalcemia. The pathophysiology may be:
- Humoral hypercalcemia of malignancy. Mediated by PTH-RP
- Squamous cell carcinomas (ie lung, esophagus)
- Cytokine induced bone release of calcium.
- Multiple myeloma
- Bone metastasis (ie breast)
Consider other etiologies if the diagnosis is not clear.
Other causes of hypercalcemia are:
- Milk alkali / calcium alkali syndrome
- Granulomatous diseases (ie sarcoidosis)
- Lymphoma
- Endocrine causes (ie. hyperthyroidism, adrenal insufficiency)
- Immobilization
Hypercalcemia Causes
Primary hyperparathyroidism
- Findings:
- Hypercalcemia with non suppressed PTH
- Evaluation:
- Look of adenoma with:
- Thyroid/ parathyroid ultrasound
- Nuclear medicine (sestamibi) parathyroid scan
- Phosphorus: Low in primary, elevated in secondary hyperparathyroidism
- 24 hour urine calcium, creatinine to calculate calcium creatinine clearance. CaCrCl
- Look of adenoma with:
(Urinary calcium x serum creatinine) / (Serum calcium x urine creatinine)
If low ( < 0.01 – 0.02) consider:
- Decreased GFR
- Familial hypercalcemic hypocalciuria
If high (> 0.02) consider:
- Primary hyperparathyroidism
- Considerations:
- In CKD/ ESRD it is not always clear. These patients may have chronic secondary hyperparathyroidism and PTH may become non suppressible. There may be another etiology for hypercalcemia or tertiary hyperparathyroidism.
- Familial Hypercalcemic Hypocalciuria. Heterozygous inactivating mutation of calcium sensing receptor.
Malignancy
- Findings:
- Hypercalcemia with suppressed PTH.
- More likely if severe hypercalcemia (calcium > 14 mg/dl).
- Evaluation:
- PTH-RP
- SPEP/UPEP/Serum free light chains
- Bone scan
- Considerations:
- Humoral hypercalcemia. Associated with squamous cell carcinoma and elevated PTH-RP
- Local cytokine release. Associated with bone metastasis (breast cancer, multiple myeloma)
Milk – Calcium Alkali Syndrome
- Findings:
- Triad of hypercalcemia (with suppressed PTH),, acute kidney injury, and metabolic alkalosis
- Evaluation:
- Typically elderly women on calcium carbonate and vitamin D for osteoporosis/osteopenia. May have baseline CKD and be on medications that affect eGFR (ie thiazides)
- Considerations:
- May be associated with severe hypercalcemia (calcium > 14 mg/dl).
- 3rd most common cause of hypercalcemia
Granulomatous Disease (i.e. Sarcoidosis/ Lymphoma)
- Findings:
- Hypercalcemia with suppressed PTH
- Evaluation:
- Elevated 1, 25 hydroxyvitamin D.
- Mediated by increased calcitriol production.
- Considerations:
- Treatment with steroids may be effective by decreasing calcitriol production.
Treatment
Treatment of hypercalcemia
- Stop offending medications
- IVF, 2-4 liters of normal saline
- It used to be said to add furosemide to enhance urinary calcium excretion. However, furosemide should be held unless volume overload is present
- Bisphosphonates –
- Require 24-28 hours for effect.
- There are concerns about potential nephrotoxicity from these meds. If abnormal eGFR give a lower dose over an extended infusion.
- Pamidronate – associated with Focal segmental glomerulosclerosis (FSGS)
- Zoledronic Acid – associated with acute kidney injury (ATN)
- Denosumab
- May be preferred over bisphosphonates if:
- Severe kidney dysfunction
- Hypercalcemia of malignancy
- Calcitonin
- Used acutely if severe hypercalcemia while awaiting bisphosphonate effect.
- Onset of action quick, but tachyphylaxis (tolerance) develops
- Steroids
- If granulomatous disease, lymphoma, or myeloma
- Cinacalcet
- Primary hyperparathyroidism with contraindication to surgery
- Dialysis
- With low calcium dialysate as an adjunctive treatment for severe hypercalcemia.
- May be preferred over bisphosphonates if:
Summary
Hypercalcemia is a condition of interest in nephrology, given its association with kidney diseases such as acute kidney injury and chronic kidney disease as well as the role of the kidney in the normal calcium, vitamin D, parathyroid axis.