Table of Contents
A fundamental principle of nephrology is this: What comes in has to go out. If more comes in than goes out or more goes out than comes in sooner or later you’re going to be in trouble.
This is how I think out too much potassium in the blood – also known as hyperkalemia
- Is it Real?
- Too Much In?
- Too Little Out?
- The Potassium is in the Wrong Place. Where’s it supposed to be anyway?
Pseudohyperkalemia
Keeping it real: What is pseudohyperkalemia?
Pseudohyperkalemia: Not real. This is when potassium leaks out of the cells after the blood is drawn. Seen with:
- Very high White blood count – like > 100K
- Very high Platelet count – like > 1M.
- Less common: Hereditary cell membrane abnormalities that make them prone to leaking potassium.
How to figure it out:
- 1st things first. Do an EKG. If it looks like hyperkalemia it probably is.
- Then: Draw a plasma or whole blood potassium, this tube does something to the blood cells that make them not available to leak potassium. It’s a Green top tube.
Other spurious causes of hyperkalemia
- Hemolysis, the cells are damaged in the process of phlebotomy causing potassium leakage. This is easy to determine if you look for it because the lab reports it.
- Excessive fist clenching with a tourniquet can cause local potassium release (from muscle cells) right at the time the blood is drawn. In this case hemolysis won’t be seen or reported, you need to question the patient.
Ok so we ruled that out, it’s real. How do we figure out what’s going on?
An approach to hyperkalemia differential diagnosis:
- Too much in
- Not enough out
- Transcellular shifts
Too much in. Ingestion or Infusion of too much potassium
This is really hard to do. Turns out the kidneys are really good at getting rid of potassium. Back in the day whenever humans (and our kidneys evolved) we weren’t stuffing our faces with salty junk food. There was a lot more potassium in the diet. The kidneys evolved to do what they had to do (excrete all that potassium). Kidneys are able to excrete much more than they need to with today’s diet and also have the capacity to upregulate potassium excretion in response to increased intake. Maybe I can see this as the cause of acute hyperkalemia, but not a good explanation for chronic hyperkalemia.
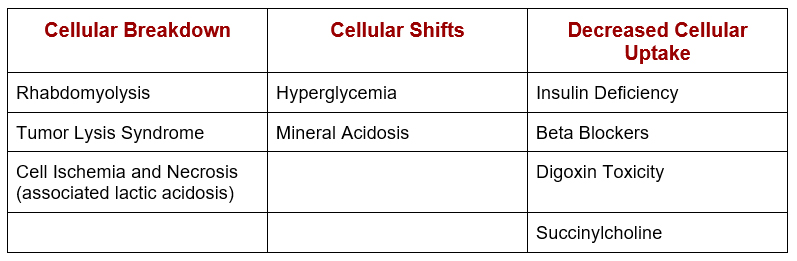
Cellular Shifts – Potassium in wrong place
Most of the body’s potassium is intracellular. States that cause potassium leakage from cells or impair potassium uptake can cause hyperkalemia. Potassium is pumped into cells via the NaK ATPase channel.
What is a mineral acidosis?
How we typically think of acidosis:
- Respiratory acidosis
- Metabolic acidosis
- Normal anion gap
- Increased anion gap
For this discussion another way to think of metabolic acidosis is:
- Mineral acidosis
- Organic acidosis
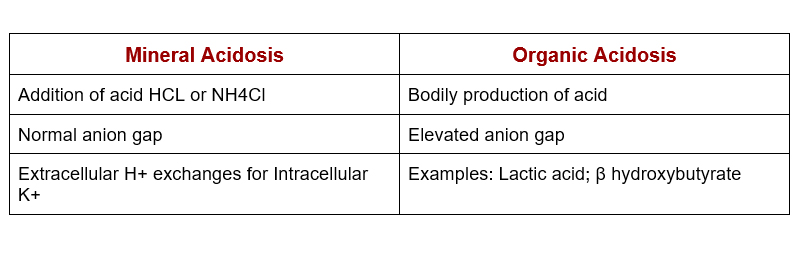
But we see hyperkalemia with lactic acidosis and diabetic ketoacidosis all the time. What’s the deal?
- The Hyperkalemia is not from the acidosis. (H+ /K+ transcellular shifts)
- Lactic acidosis: Hyperkalemia is from cellular ischemia/necrosis
- Diabetic ketoacidosis Hyperkalemia is from insulin deficiency +/- osmotic gradient from hyperglycemia.
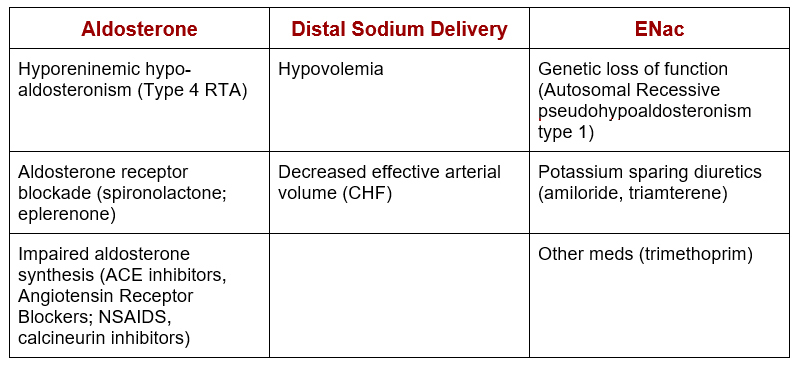
Not enough out
This is where the money is. There are two fundamental reasons why the kidneys won’t excrete enough potassium.
- A problem with aldosterone or
- A problem with sodium delivery to the distal nephron or
- A problem with the epithelial sodium (ENac) channel
All causes come down to this. Low GFR (CKD) by itself is not a good explanation unless the GFR is really low (like ESRD). If the GFR is 0 then there’s no sodium getting to the distal nephron, but for pre ESRD CKD the kidneys should be able to excrete enough potassium if there isn’t a problem with aldosterone or distal sodium delivery.
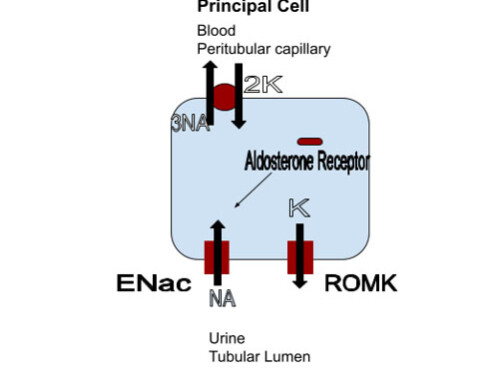
How do the kidneys excrete potassium? The principal cell in the distal nephron. The distal nephron has principal and intercalated cells. I think about it like this, the kidney principally wants to hang on to sodium. So the principal cells have epithelial sodium (ENac) channels. These absorb sodium into the cells, creating an electrochemical gradient for potassium secretion through those channels (ROMK and MAXI K). Aldosterone upregulates these ENac channels.
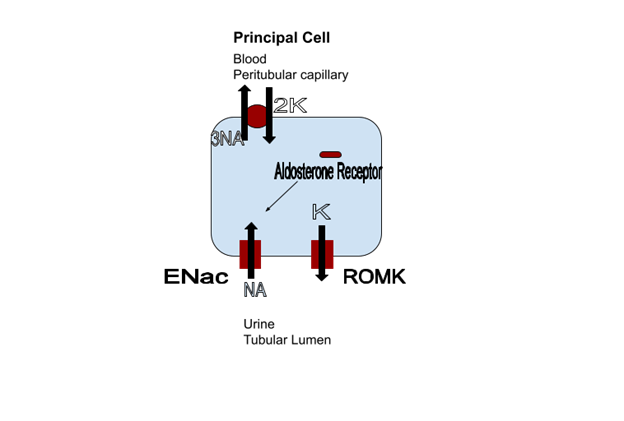
So:
Aldosterone
Problem with aldosterone = not enough ENac channels = not enough sodium resorption = not enough electrochemical gradient = not enough potassium secretion.
Distal tubular sodium delivery
Problem with distal tubular sodium delivery = not enough sodium getting to where the ENac channels are at = not enough sodium resorption = not enough electrochemical gradient = not enough potassium secretion.
Epithelial sodium (ENac) channel
Problem with epithelial sodium (ENac) channel = sodium can’t get resorbed = not enough electrochemical gradient = not enough potassium secretion.
It’s a brilliant system really. If the body is low on sodium, then less will get to the distal nephron, aldosterone synthesis is increased leading to upregulation of ENac channels. If the body has too much sodium, there is a lot of distal delivery and the body downregulates aldosterone synthesis. For a problem to occur this normal counterbalance mechanism is off.
Summary
There’s the framework on how to think about hyperkalemia:
- Is it real
- Too much in
- Transcellular shifts
- Too little out
- Problem with sodium delivery to distal tuvalu
- Problem with ENac
- Problem with aldosterone