Table of Contents
What is glomerulonephritis?
Glomerulonephritis is inflammation of the glomerulus. This is may be manifest by:
Clinical Findings:
- Glomerular hematuria
- Variable proteinuria (typically sub nephrotic may be nephrotic)
- Leukocyturia (variable)
- Impaired kidney function (variable)
- Hypertension (variable)
- May be renal limited or associated with systemic inflammation (vasculitis)
Pathologic Findings:
- Glomerular hypercellularity
- Crescents (indicate more severe glomerular inflammation)
The clinical course may be indolent with slowly progressive CKD, acute and self limited, or fulminant with progressive deterioration of kidney function over days, weeks, or months. The latter clinical presentation is referred to as Rapidly Progressive Glomerulonephritis (RPGN). This is often associated with extensive crescents involving > 50% of glomeruli.
When do we consider glomerulonephritis?
We worry about glomerulonephritis in 3 situations:
Acute or subacute worsening kidney function, with other signs of glomerular disease.
- Proteinuria (often subnephrotic)
- Leukocyturia
- Hypertension
- Edema
Systemic signs suggestive of vasculitis
- Rash (ie palpable purpura)
- Inflammatory arthritis
- Pulmonary hemorrhage
Hematuria
The hallmark of glomerulonephritis is glomerular hematuria
What is glomerular hematuria?
It’s hematuria that comes from the glomerulus as opposed to from another lesion in the GU tract (kidney, ureter, or bladder). How do we tell?
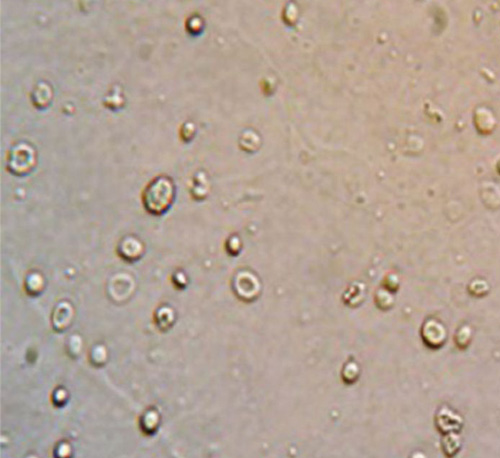
- Dysmorphic red blood cells. Nonglomerular hematuria is typically monomorphic (smooth round shape). Glomerular hematuria has misshapen (dysmorphic RBCs). It is said that if >40% of RBCs are dysmorphic, defines glomerular hematuria. (these can be counted under phase microscopy)
- Acanthocytes are a classic type of dysmorphic RBC which have blebs, like Mickey Mouse ears. If > 5 % RBCs are acanthocytes (under phase microscopy) defines glomerular hematuria.
- Red Blood Cell casts. A cast with RBCs in it. Having even 1 RBC cast on a low power field defines glomerular hematuria.
Bottom line.
If there is hematuria (> 5 red blood cells per high power field) and you see a RBC cast or acanthocytes there is glomerular hematuria
What is the pathophysiology of glomerulonephritis?
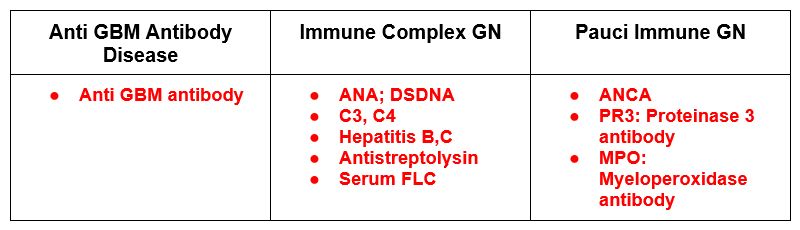
When glomerular hematuria is present we are concerned about 3 potential pathophysiologic mechanisms present.
-
Antibodies against the glomerular basement membrane
- Anti GBM antibody disease (Goodpasture’s)
-
Immune complexes that deposit in the glomeruli causing inflammation
- Cryoglobulinemia
- IgA Nephropathy
- Lupus Nephritis
- Membranoproliferative Glomerulonephritis
- Post Streptococcal/Infectious GN
- PGNMID: Proliferative Glomerulonephritis with Monoclonal Immunoglobulin Deposits
-
Pauci Immune: ANCA associated
- Granulomatosis with polyangiitis (GPA) – C ANCA
- Microscopic polyarteritis (MPA) – P ANCA
- Churg Strauss syndrome
TIP
There are some renal conditions that may be associated with glomerular hematuria, but are not glomerulonephritis. These may be considered if a proliferative glomerulonephritis is not present.
These include:
- Diabetic Nephropathy. This is a glomerulopathy not a glomerulonephritis. We typically see proteinuria, but microscopic glomerular hematuria may also be present.
- Warfarin (anticoagulant associated) Nephropathy
- Thin Basement Membrane Disease. Benign Familial Hematuria
- Alport’s Syndrome
- Atheroembolic Renal Disease
What is the evaluation of suspected glomerulonephritis?
There are two components to evaluation:
- Serologic evaluation
- Renal biopsy
The serologic evaluation is based on the above Diagnostic classification:
Renal Biopsy will be required for diagnosis in most cases. Light microscopy will show proliferation often with crescents and may not distinguish the cause.
The diagnosis is made on Immunofluorescence
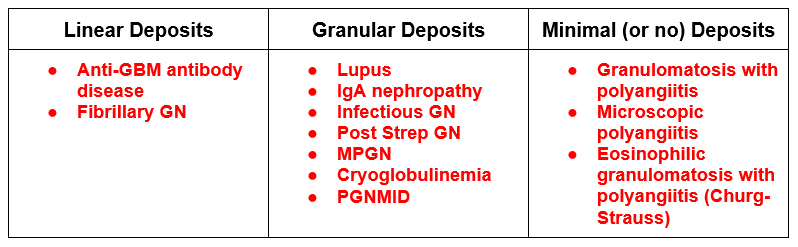
- Anti GBM antibody disease will have linear staining with IgG and C3. This is because the antibody is against the basement membrane itself so the deposition is continuous.
- Immune Complex will have granular deposition. (Often IgG and C3). This is because the pathogenesis is antibody-antigen complexes that deposit in the glomerulus in a non continuous pattern.
- ANCA associated with have negative or minimally positive immunofluorescence, this is not associated with immune complex deposition and there is a paucity of staining
Summary
Glomerulonephritis is inflammation of the glomerulus and is important to recognize as it may be associated with a decline in kidney function. The hallmark is glomerular hematuria and it may be renal limited or part of a syndrome with systemic inflammation. Prompt diagnosis often requires a serologic evaluation and kidney biopsy.




Thanks! Let me know what future topics would be of interest to you.