Table of Contents
FSGS is a pathologic description meaning a part (segment) of some of the glomeruli (focal) are scarred (sclerosis). Since scarring is the end result of most glomerular injury, anything that is severe enough for long enough will end up causing sclerosis.
It’s like minimal change disease, but worse. It is a more common cause of nephrotic syndrome in adults (less common in children). 20-30% adults with nephrotic syndrome will have FSGS.
How is it like minimal change disease?
- It is manifest by damage to podocytes
- Primary/ Idiopathic and some causes of secondary FSGS present as full nephrotic syndrome
How is worse than minimal change disease?
- Less responsive to steroids and more likely to be steroid resistant
- More likely to result in progressive CKD and progress to ESRD
Makes sense, I think about it like this. Minimal change disease is not severe enough to cause scarring in the glomeruli while FSGS is.
Approach to Diagnosis
FSGS is diagnosed by kidney biopsy. So you have a patient with proteinuria and you get a kidney biopsy. The pathology shows FSGS. You’re done with the diagnosis right?
Nope, you’re just getting started.
What we need to deduce is the underlying pathologic state that caused the pathology finding. What is causing damage to the podocytes? This will determine the appropriate course of treatment.
One of the cool things about nephrology is you get to talk with pathologists. Sounds weird lol. The clinical history is critical for a nephropathologist to make an accurate diagnosis. For this reason nephrologists and nephropathologists often discuss the clinical case and pathological findings directly when coming to a diagnosis.
When the pathology shows FSGS here’s what you need to deduce. Is it?
- Primary idiopathic FSGS – A circulating permeability factor causes damage to the podocytes.
- Secondary FSGS – A virus, toxin, or sheer stress causes damage to the podocytes.
- Genetic FSGS
- Residual scarring from prior inflammatory glomerular disease.
Why is this important?
We need to figure out which patients will benefit from immunosuppression and which not so we can avoid unnecessary risk.
Primary idiopathic FSGS is most likely to benefit from immunosuppression. Genetic FSGS may respond to immunosuppression, but is often steroid resistant. Secondary FSGS and Residual Scarring do not benefit from immunosuppression and of course immunosuppression carries risk.
Primary Idiopathic FSGS
Primary idiopathic FSGS is an immunologic condition of unknown etiology that causes nephrotic syndrome. Like Minimal Change Disease it is considered a podocytopathy. There is a postulated circulating permeability factor that causes damage to the podocyte with resultant proteinuria and nephrotic syndrome.
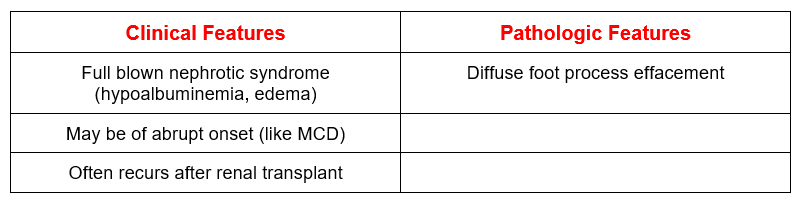
This is the type that is more likely to benefit from immunosuppression.
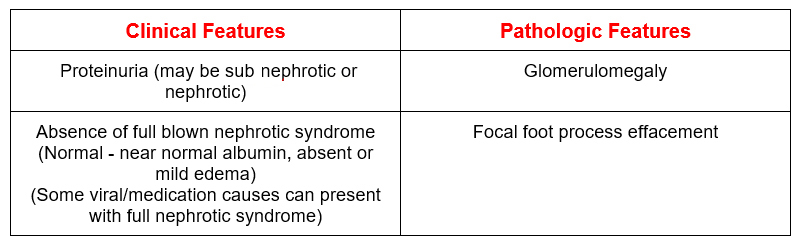
Secondary FSGS
Secondary FSGS often does not present as full blown nephrotic syndrome even if there is nephrotic range proteinuria.
Causes of Secondary FSGS
- Viral – Infection of podocyte
- Drugs – Toxicity to podocyte
- Hyperfiltration/Adaptive – Mechanical strain/ shear stress to podocyte
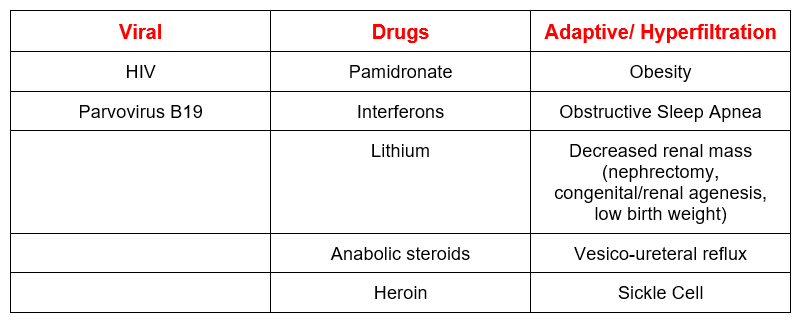
Immunosuppression is unlikely to help and steroids may not be a good idea in patients with obesity and/or obstructive sleep apnea. Treatment focuses on addressing underlying secondary cause and Renin Angiotensin Aldosterone System (RAAS) blockers.
Genetic FSGS
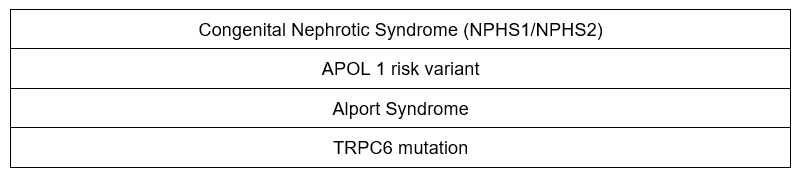
The latter 3 you may see in adults. Often steroid resistant. Calcineurin inhibitors (cyclosporine or tacrolimus) may be tried with some success.
Residual scarring
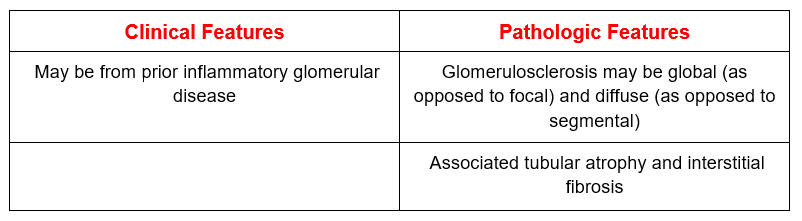
Avoid immunosuppression. Treat with Renin Angiotensin Aldosterone System (RAAS) blockers.
Treatment
The options are the same as those for minimal change disease.
- Steroids
- Calcineurin inhibitors (cyclosporine or tacrolimus)
- Mycophenolate Mofetil
- Cyclophosphamide
- Rituximab
How I treat FSGS
Remember immunosuppression is only indicated in Primary/Idiopathic and some cases of genetic FSGS
- Calcineurin inhibitors (cyclosporine or tacrolimus). I go straight to this option. The guidelines suggest using high dose prednisone (1 mg/kg up to 80 mg a day) for up to 4 months. I am not a fan. I find that a regimen with a calcineurin inhibitor and low dose prednisone is much better tolerated.
- Cyclosporine: 3-5 mg/ kg day (divided in 2 doses, dosed q 12 hrs with target trough 100-175)
- Tacrolimus: 05-0.1 mg/kg day (divided in 2 doses, dosed q 12 hrs with target trough 5-10)
- Use along with low dose prednisone (0.15 mg/kg/day). This dose of prednisone (typically 15 mg per day) is better tolerated than 60 mg per day.
- Long regimen (prone to relapse when they are weaned). Therefore the regimens are longer. The initial dose for 12 months, wean over another 6-12 months.
For patients who don’t respond to this regimen, the options are:
- Mycophenolate Mofetil (regimen as above)
- Cyclophosphamide (see below for regimen)
- Rituximab (see below for regimen)
For patients who relapse. Here are your options:
- Repeat course of calcineurin inhibitor.
- Cyclophosphamide: In my experience this medication is perhaps the most likely to result in a durable remission for glomerular diseases.
- Rituximab:
Recurrence post renal transplant
- Plasmapheresis
- Rituximab
Summary
FSGS is a more common, more severe and more difficult to treat condition than minimal change disease. The key is to understand the underlying pathophysiologic to determine which patients will benefit from immunosuppression.



