Table of Contents
Dialyzers are where dialysis, the blood purification takes place. This article will address:
- Dialyzer Components
- Types of Dialysis Membranes
- Sterilization Techniques
- Dialyzer Reactions
Dialyzer Components
Dialyzers are composed of an outer capsule or shell in which the membranes are located.
Capsule / Shell
There are 2 components to the capsule/ shell in which the dialysis membranes are located.
- Housing: The outer cylinder
- Polycarbonate
- Polypropylene
- Potting: What holds the dialysis membranes in place at both ends of the dialyzer.
- Polyurethane
Membranes
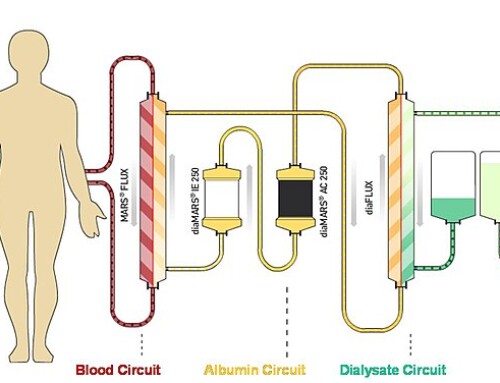
Hollow fiber dialysis membranes are located within the capsule. They are bathed in the dialysate fluid which flows through. Blood flows through the hollow fibers in a countercurrent direction. Diffusion occurs through these semipermeable membranes.
The composition and sterilization of these dialysis membranes are critical as the patient’s blood is exposed to them throughout the dialysis procedure.
Types of Dialysis Membranes
- Cellulose (cuprophran): Unmodified cellulose was the 1st generation dialysis membrane. This was a cotton derivative. Exposure of blood to these membranes, specifically the free hydroxyl groups, leads to inflammation resulting in activation of the alternate complement cascade. This makes them bioincompatible. Not used currently (at least in US)
- Substituted/ modified cellulose: Reduced complement activity increasing biocompatibility
- Cellulose acetate, diacetate, triacetate: Free hydroxyl group replaced by acetate
- Hemophan: Synthetic material added to cellulose during production
- Synthetic: Most biocompatible
- Polysulfone
- PMMA: Polymethylmethacrylate
- Polyethersulfone
- PAN: Polyacrylonitrile
Synthetic membranes (i.e. Optiflux; Revaclear) are the most common dialyzers in the US. Modified cellulose (i.e Nipro Cellentia) are also used.
Biocompatibility
Contact of blood with the dialysis membrane causes an inflammatory reaction activating complement. Membranes that are less biocompatible have an increased incidence of this. This results in:
- Neutropenia: Neutrophils are sequestered in the pulmonary circulation resulting in transient neutropenia. The neutrophil count nadirs at 15 minutes, subsequent bandemia (lasting up to 5 hrs) normalizing the WBC.
- Transient Lymphocytopenia and Thrombocytopenia may occur
- Type B dialyzer reaction.
Historically dialysis patients had these membranes reprocessed and reused for a number of dialysis sessions. Although this was done for expense, with reuse the membranes were coated with plasma proteins and reactions were abated. This led to the terminology “first use syndrome”.
Reuse of dialyzers is not currently practiced in the US.
Modified cellulose and synthetic dialyzers are progressively more biocompatible reducing the incidence and severity of dialyzer reactions, although they still may occur.
Sterilization
Dialyzers need to be sterilized as the patient’s blood is exposed to them. There are different methods of sterilization including:
- Ethylene oxide
- Electron Beam CT (EBCT)
- Gamma irradiation
- Steam
Ethylene Oxide is associated with IgE mediated (Type A) allergic reactions. For this reason it is less commonly used currently.
EBCT is associated with thrombocytopenia.
Dialyzer Reactions
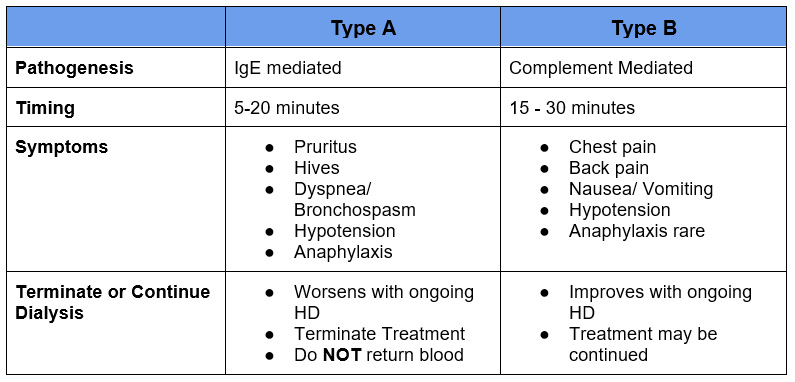
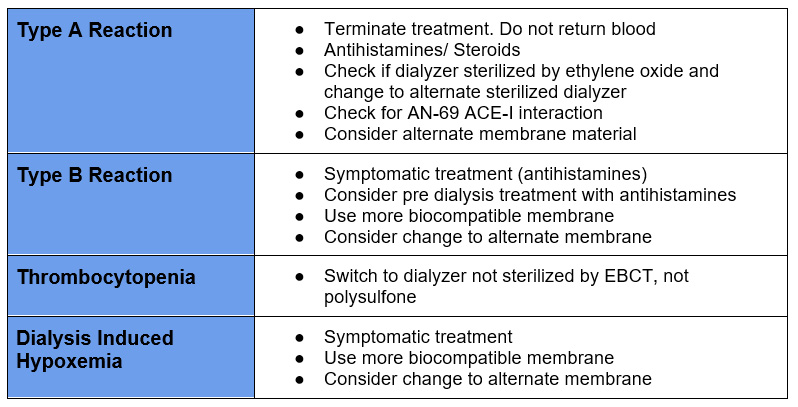
Type A
- These are more severe allergic reactions may progress to anaphylaxis
- Occur in 1st few minutes of dialysis treatment
- Eosinophilia may be a risk factor
- Dialysis should be terminated immediately and the blood in the dialysis circuit should NOT be returned to the patient
- Associated with ethylene oxide sterilant
- Differential:
- AN-69 membranes in patients on ACE-inhibitors (activates bradykinin)
- PAN membranes are pretreated resulting in marked reduced bradykinin production
- Medication reactions (heparin, IV iron)
Type B
- Less severe reactions
- Occurs later in dialysis session
- Dialysis may be continued
- Occurs with less biocompatible membranes
It is not uncommon that patients may have milder type B symptoms or pruritus even with biocompatible synthetic membranes. Polysulfone membranes can activate complement, but the complement is reabsorbed limiting the symptoms. Synthetic membranes may also cause IgE mediated effects. Although it is often not clear if the symptom is coincident or caused by dialyzer it is reasonable to try an alternate dialyzer.
Thrombocytopenia
Does Dialysis Cause Thrombocytopenia? @BCNephro – YouTube
- Usually this mild and transient with platelet counts rebounding prior to the next dialysis session.
- Common with less biocompatible cellulose membranes
- More severe and progressive thrombocytopenia can occur with current synthetic biocompatible membranes. Associated with:
- EBCT sterilization
- Polysulfone membranes – although more biocompatible may have platelet activating capacity
It is hard to sort out as many polysulfone dialyzers are also sterilized by EBCT.
It is ironic as in these cases the more biocompatible dialyzer is changed to a less biocompatible Cellulose Triacetate dialyzer (sterilized by gamma irradiation).
These articles report dialyzer related thrombocytopenia.
Intradialytic Hypoxemia
- Intradialytic hypoxemia may occur. This is counterintuitive as fluid removal would be expected to relieve pulmonary congestion and improve oxygenation.
- Often attributed to comorbidities, CHF, COPD, OSA
- May be symptom of dialyzer reaction via pulmonary sequestration of neutrophils
Treatment
Summary
Dialyzers are composed of membranes of different synthetic material and varying degrees of biocompatibility. There are different sterilization techniques. Dialysis reactions may be complement mediated from less biocompatibility or allergic IgE mediated. Consider these reactions in addition to infectious and cardiovascular etiologies when evaluating symptoms on dialysis.