Table of Contents
Mineral bone disease in dialysis patients refers to assessment and management of Phosphorus, Calcium, and Parathyroid Hormone (PTH)
Pathophysiology
The kidney normally is responsible for excretion of phosphorus and conversion of inactive – 25- hydroxyvitamin D to active – 1,25-hydroxyvitamin D via the enzyme 1 alpha-hydroxylase.
Therefore with kidney failure there is:
- Impaired phosphorus excretion causing hyperphosphatemia. This results in an increase in parathyroid hormone and FGF 23 in an attempt to increase phosphorus excretion. However, the kidneys do not work so this is ineffective.
- Hyperphosphatemia contributes to vascular calcification and is associated with an increased cardiovascular mortality. Link – Impact of longer term phosphorus control on cardiovascular mortality in hemodialysis patients using an area under the curve approach: results from the DOPPS
- The increase in PTH affects the bone and can cause high turnover bone disease (osteitis fibrosa cystica).
- Impaired production of 1,25 Vitamin D. This leads to decreased GI enteric calcium absorption which also contributes to PTH elevation (in an attempt to maintain normocalcemia).
Management
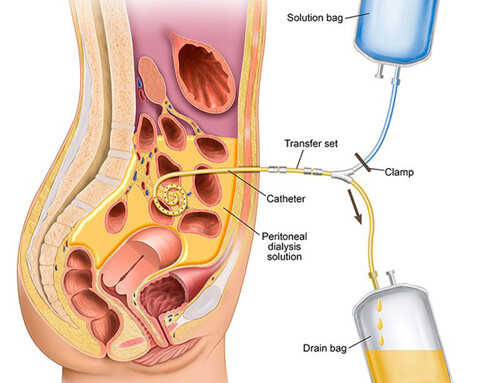
Phosphorus
Patients with ESRD therefore tend to have hyperphosphatemia which can result in vascular calcification with increased cardiovascular mortality and contributes to PTH elevation. Although dialysis removes phosphorus, standard dialysis is insufficient to maintain neutral phosphorus balance. Daily or extended (nocturnal) dialysis does a better job of this.
The target phosphorus in dialysis patients is 3.5-5.5.
Treatment to maintain this target include:
- Diet: Many foods (including protein) contain phosphorus. The idea is for patients to avoid foods that are high in phosphorus that are not of high biologic value. Patients are typically counseled to avoid.
- Dairy products
- Colas (dark sodas). These are preserved with phosphoric acid. Clear sodas are preserved with citric acid.
In addition the phosphorus in processed foods is more absorbed than that in whole foods.
Links to dietary phosphorus resources for patients.
Low Phosphorus Diet for Kidney Disease Patients
Phosphorus and Your Diet – Levels, diet, deficiency | National Kidney Foundation
- Phosphorus Binders: Restriction of dietary phosphorus is important, but typically not sufficient to control phosphorus. Therefore phosphorus binding agents are also required. Phosphorus binding agents include:
Aluminum hydroxide (amphojel): This was a historical phosphorus binder. However, it ended up causing complications of aluminum toxicity:
Anemia, dementia, and bone disease (osteomalacia)
For this reason it is not currently used as a binder.
Tip:
Sucralfate (used as adjunctive therapy for peptic ulcer disease contains aluminum. Its use can result in hypophosphatemia and chronic use in aluminum toxicity in patients with ESRD. Chronic use should be avoided.
Calcium containing:
Calcium acetate (Phos-Lo) – The most common calcium containing phosphorus binder. Purported to be more effective than calcium carbonate (however may have a higher incidence of intolerance.
Calcium carbonate (Os-cal/Tums) – I advise patients to take this is they have problems getting their prescription binder covered or filled.
Hypercalcemia and concerns about positive calcium balance and vascular calcifications can limit the use of calcium containing phosphorus binders. It is advised to not go higher than 9 pills of calcium acetate daily.
Non calcium phosphorus binders: There are currently four available.
- Sevelamer carbonate (Renvela)
- Pill and powder form
- Lanthanum carbonate (Fosrenol)
- Chewable tablets
- Concerns of potential toxicity similar to aluminum have not panned out
- Ferric citrate (auryxia)
- Increases iron store
- Sucroferric oxyhydroxide (Velphoro)
- Chewable
Calcium
Target corrected calcium: < 9.5 mg/dl
Although there is a tendency toward hypocalcemia with decreased GFR, there is a concern of positive calcium balance, elevated calcium phosphorus product (calcium x phosphorus) and vascular calcifications. Therefore mild asymptomatic hypocalcemia (calcium > 7.5 mg/dl) should not be treated.
Dialysate: Standard calcium bath is 2.5 meq/Liter. A 3.0 meq/Liter bath is also available. I prefer to avoid the higher calcium dialysate (unless symptomatic ie. post parathyroidectomy) to help mitigate this positive calcium balance.
Hypocalcemia etiologies:
- Iatrogenic from the calcimimetic agents (cinacalcet/parsabiv).
- Post parathyroidectomy as manifestation of hungry bone syndrome.
Hypercalcemia etiologies:
- Iatrogenic from calcium containing phosphorus binders and vitamin D analogs.
- Tertiary hyperparathyroidism. Chronic stimulation of the parathyroid gland can be associated with decreased responsiveness to negative inhibition from calcium or active vitamin D
Parathyroid Hormone (PTH)
Target PTH in ESRD is 2-9 times upper limit of normal (100 – 600 pg/ml). This is because the PTH assay blood test also measures some inactive metabolites (which tend to accumulate with decreased GFR). Therefore a “normal” PTH level is not appropriate for ESRD patients. A “normal” PTH in an ESRD patient is often associated with low turnover bone disease and hypercalcemia.
Treatment
Vitamin D (ergocalciferol vitamin D2; cholecalciferol vitamin D3)
- These are essentially the same (D2 is plant based; D3 is animal based or from the sun).
- Necessary to provide sufficient vitamin D substrate to be available for conversion to 1,25 vitamin D.
- Assessed by 25 vitamin D levels ( Target >30)
Active Vitamin D
- Calcitriol (1,25 vitamin D) – biologic active form.
- Paricalcitol (Zemplar) – vitamin D analog
- Doxercalciferol (Hectorol) – vitamin D analog.
These suppress PTH, but also increase GI calcium and phosphorus absorption and therefore may contribute to hypercalcemia and hyperphosphatemia. The analogs supposedly have a greater affinity for the parathyroid receptor than GI receptors and be less likely to result in hypercalcemia or hyperphosphatemia. However, they are not convincingly better and calcitriol has become the most common form of active vitamin D used by dialysis providers.
Calcimimetics
-
- Cinacalcet (Sensipar)
- Oral formulation
- Given post hemodialysis (removed by dialysis)
- Etelcalcetide (Parsabiv)
- IV formulation
- Given with dialysis (if intolerance to oral formulation).
- Cinacalcet (Sensipar)
Parathyroidectomy
-
- This may be necessary with hyperparathyroidism refractory to treatment especially if complications of high turnover bone disease or calciphylaxis
- Less common with advent of calcimimetics
- 4 gland parathyroidectomy typically performed.
- Significant 30 day and 1 year mortality. Hypocalcemia from hungry bone syndrome may be life threatening (cardiac arrhythmias).
My concern regarding parathyroidectomy is this. Nonadherence with phosphorus binders with chronic uncontrolled hyperphosphatemia is often a contributor to hyperparathyroidism severe enough to warrant parathyroidectomy. These same patients need to be adherent with calcium supplements and calcitriol post operatively to prevent life threatening hypocalcemia from hungry bone syndrome.
Summary
Mineral Bone Disease management in ESRD patients is not only important to prevent complications of bone disease, but also to prevent vascular calcifications and improve cardiovascular mortality.