Table of Contents
It has become more common for patients with dialysis requiring acute kidney injury (AKI) to be dialyzed in the outpatient setting. With more medically complex patients and the incentive to decrease length of hospitalizations it is not uncommon for patients with dialysis requiring AKI to be discharged from the hospital prior to recovery of kidney function.
Traditionally outpatient dialysis was intended for patients with End Stage Kidney Disease. Nephrologists would attest that the kidney failure is permanent and irreversible by signing a form called a 2728.
The evolution has allowed a mechanism for patients with dialysis requiring AKI to receive hemodialysis in an outpatient center after hospital discharge. This transition of care requires special considerations.
This article will address:
- How to predict likelihood of recovery of kidney function
- How to monitor for recovery of kidney function
- How to determine when AKI has become End Stage Kidney Disease
How to predict likelihood of recovery of kidney function
Presence and Severity of CKD
The main determinant is the presence and severity of chronic kidney disease (CKD) prior to the episode of AKI.
- If the kidney function was normal prior to the AKI episode, I would expect recovery.
- If the patient had late stage CKD (ie CKD stage 4), recovery would be less likely. This is particularly true if there are comorbidities and concomitant difficulties managing hypervolemia as in congestive heart failure..
Cause of AKI
The cause of AKI that can provide useful information.
- Acute tubular Necrosis (ATN) would be more likely to recover kidney function than an untreated rapidly progressive glomerulonephritis (RPGN).
- The chronicity seen on kidney biopsy (which is best assessed by tubulointerstitial fibrosis and tubular atrophy) can also be a predictive factor.
Duration of AKI
- The longer someone requires dialysis (especially if they are oligo-anuric), the less likely there will be recovery of kidney function
How to monitor for recovery of kidney function
There are 2 things necessary to not require ongoing dialysis
- Sufficient kidney function (glomerular filtration rate GFR) to avoid uremic complications.
- Sufficient urine volume to maintain an acceptable steady state volume status, ideally euvolemia.
Assessing kidney function (GFR)
The limitation here is that these assessments use a serum creatinine. The creatinine is not in steady state in a patient with kidney failure. That is the serum creatinine immediately after dialysis will be much lower than immediately before the next dialysis.
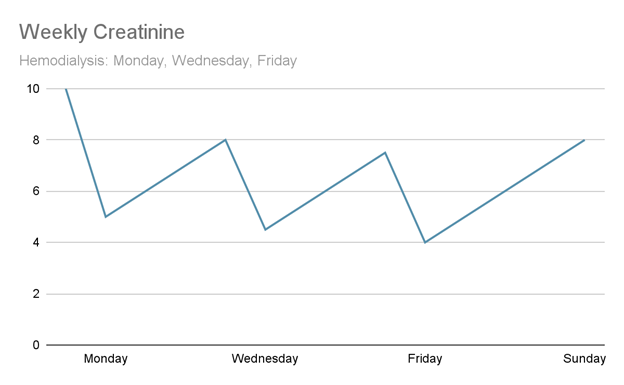
There is a way to use a time averaged creatinine, but my approach is be conservative and use the pre dialysis creatinine prior to the first treatment of the week (Monday or Tuesday).
The methods to assess kidney function are:
- Interdialytic urine collections (which tend to be around 48 as opposed to 24 hrs) to calculate GFR. This information may be useful, but I find it difficult and sometimes misleading for the following reasons.
- It is cumbersome and difficult to know if the collection is accurate.
- To measure a GFR (as opposed to a creatinine clearance) the creatinine clearance (which may overestimate GFR due to tubular secretion) and urea clearance are averaged.
- Use of a timed average pre dialysis and post dialysis creatinine (given creatinine fluctuations as highlighted above). I worry that this may lead to an overestimate.
As noted above, when using this method I make my calculations using the predialysis creatinine only. This is a conservative (worst case scenario) estimate to determine if the patient can fly without dialysis.
- Trend the pre-dialysis creatinine over the long dialytic interval (Monday or Tuesday) weekly. This is my preferred method.
- If the weekly pre-dialysis creatinine is trending down to a reasonable level (ie< 4 mg/dl), this is a sign that there may be enough renal recovery to come off dialysis.
Assessing sufficient urine volume
Although an interdialytic 24 or 48 urine collection will provide urine volume, it cannot necessarily inform if the urine volume is adequate. What is more informative?
- Interdialytic weight gain
- Physical exam (presence of edema)
Bottom line:
When dialysis is discontinued in the outpatient setting close monitoring is required. The recovery for the AKI may be incomplete and the patient may have significant residual CKD. They may have concomitant conditions (such as heart failure) that increase the risk of hypervolemia.
This is often difficult to do logistically as the patient may have challenges getting to the office clinic and the clinic may be too busy to meet those needs. How I deal with these challenges is by weaning dialysis.
My algorithm
- Trend weekly pre-dialysis creatinine until it improves to a level where dialysis is not expected (i.e. a stage 4 CKD eGFR range).
- Ensure that interdialytic weight gains are not excessive (use loop diuretics if necessary).
- Wean dialysis from three times to twice a week.
- Ensure that the patient remains stable from a lab and volume standpoint.
- Wean dialysis from twice to once a week.
- Ensure that the patient remains stable from a lab and volume standpoint.
- Stop dialysis
- Check labs (BMP) 1 week after dialysis discontinuation.
- Ensure that the labs remain stable.
- Arrange for dialysis catheter removal.
This process can be quite accelerated (over 1-2 weeks) in a patient with complete recovery to normal kidney function and little to no interdialytic weight gain (or interdialytic weight loss). It may be prolonged in a patient whose recovery of kidney function is slower and/or has ongoing significant interdialytic weight gains.
How to determine when AKI has become End Stage Kidney Disease
The most straightforward way is 90 days. If the patient still requires dialysis after 90 days it is unlikely (although not impossible) that recovery will recur and is appropriate to classify them as End Stage Kidney Disease (ESRD).
The original AKI staging criteria RIFLE, which was a precursor to the current AKI staging criteria, used the E for End stage kidney disease – defined as kidney failure lasting greater than 90 days.
This is important for several reasons including:
- Dialysis access (fistula or graft) planning can occur.
- Kidney transplant evaluation can occur.
Summary
Outpatient dialysis for patients with AKI has become more common. The associated transitions of care – from hospital to dialysis clinic and dialysis clinic to outpatient CKD clinic can be challenging. Trending weekly pre-dialysis creatinine, monitoring interdialytic weight gains, and weaning dialysis can be useful methods to address these challenges.