Table of Contents
Arteriovenous access is the preferred access for hemodialysis (as opposed to use of a catheter).
There are 2 types of arteriovenous access
- Arteriovenous fistula (AVF) – native artery transposed to native vein. Native vein hypertrophies under increased arterial pressure. This becomes fistula. This is the preferred dialysis access (over both catheters and arteriovenous graft). As it is native tissue it is least likely to thrombose and least likely to become infected.
- Arteriovenous Graft (AVG) – Synthetic material used as a conduit connecting. Preferred over catheter, but less preferable than arteriovenous fistula.
Types of Fistulas and grafts
AVF – Fistulas
- Radiocephalic: Radial artery to cephalic vein. Located at wrist (base of thumb)
- Brachiocephalic: Brachial artery to cephalic vein. Located in upper arm (elbow)
- Basilic vein transposition: Brachial artery to basilic vein. Basilic vein is deep and needs to be transposed to the surface to allow cannulation. Located in the upper arm.
AVG – Grafts
- Looped forearm: Brachial artery to brachial or cephalic vein.
- Straight forearm: Radial artery to cephalic vein.
- Straight upper arm: Brachial artery to axillary vein.
- Looped upper arm: Axillary artery to axillary vein.
How do you tell the difference between a fistula and a graft? Read here.
Fistulas and Grafts: Advantages and Disadvantages
Arteriovenous Fistulas
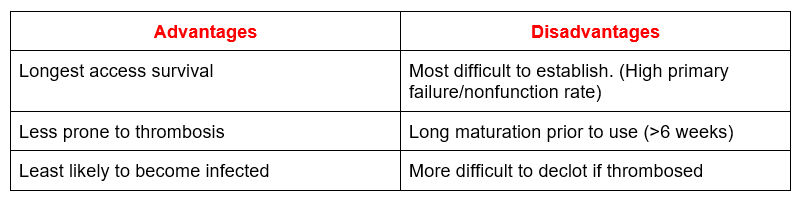
Fistulas require sufficiently large and healthy vessels to be feasible. For this reason vein mapping is recommended prior to access placement. In patients with chronic kidney disease approaching the need for dialysis it is recommended that a fistula be placed > 6 months before it is anticipated dialysis will be required. If this type of access does thrombose it is important to attempt a thrombectomy and perform a fistulogram promptly.
Arteriovenous Grafts
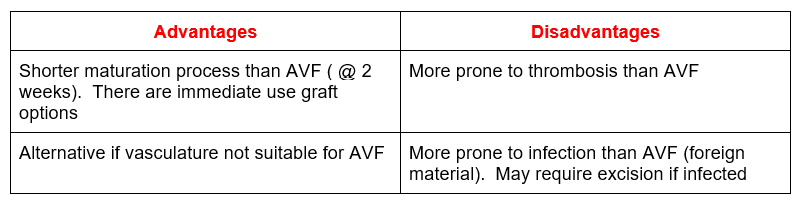
In patients with chronic kidney disease approaching the need for dialysis it is recommended that a graft be placed > 3-6 weeks before it is anticipated dialysis will be required. May be more appropriate in older patients on dialysis with shorter life expectancy as shorter maturation process will allow for shorter duration of catheter use.
Do vein mapping (typically by ultrasound) prior to access placement to assess if anatomy is suitable for AVF vs AVG.
Evaluation and Monitoring
How to assess access
- Presence of bruit and thrill. This tells you if access is patent, if there is flow. The flow should be of a continuous whirring type nature. If it is pulsatile it indicates a dysfunctional access. This suggests a venous or outflow stenosis, resulting in back pressure.
The presence of a bruit/ thrill is sufficient to determine that a graft can be cannulated, but it does not mean the fistula is adequate for use. To assess if a fistula is adequate for cannulation look and feel its size. If it looks large enough for a nurse to be able to get 2 large bore needles into it, it’s adequate for use. For this assessment you can use a tourniquet (like one used for phlebotomy). But, don’t use a tourniquet on a graft, this can cause it to thrombose.
- Other physical findings
- Arm edema
- Collateral veins
- If you raise the arm, the fistula should collapse.
- Look for areas of dilatation (aneurysms in AVF or pseudoaneurysms in AVG
How dialysis access (fistula) are cannulated
- Rope ladder technique: (Puncture sites are rotated each dialysis session)
- Buttonhole technique: (Same site is used. A tract is created using a sharp needle, these tracts are subsequently accessed with a blunt needle). This technique is sometimes used for home or frequent (ie daily or near daily dialysis). The benefits of this technique are less pain and that it is easier for self cannulation. There is a concern for an increased risk of infection. Post dialysis the tracts form scabs that need to be adequately removed and the site disinfected prior to the next cannulation.
Monitoring of Access function
- Clinical:
- Physical examination findings (pulsatile)
- High venous or low arterial pressures
- Difficulty with cannulation
- Increased bleeding post dialysis
- Ultrasound (transonic flow)
- Low flow
- Decrease in flow of > 25% from baseline
These findings suggest a venous outflow or central stenosis. These are risk factors for access thrombosis. Detection and intervention with a fistulogram by interventional nephrology or radiology can prevent thrombosis. This is ideal as it may result in decreased hospitalizations and missed treatments.
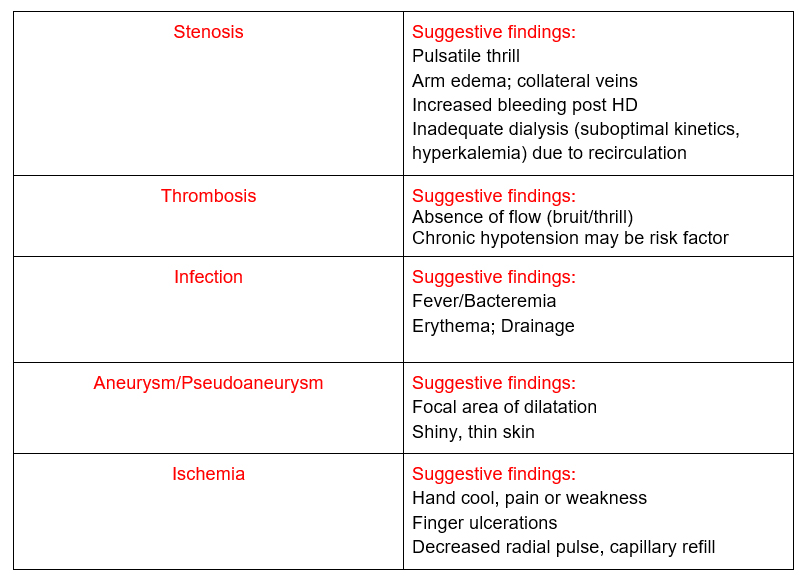
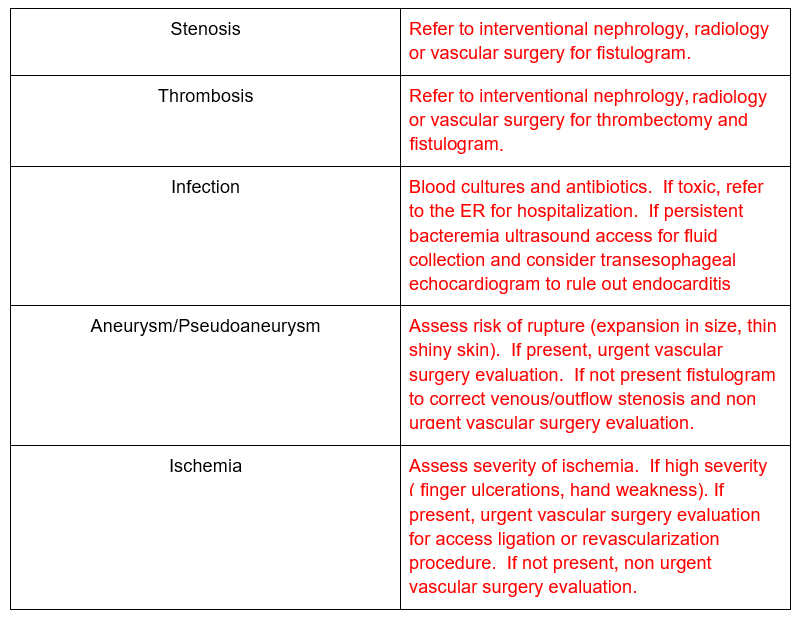
Complications
Interventions
Summary
Arteriovenous access is crucial for hemodialysis. AVF are preferred although there may be times where AVG are necessary. Adequate preparation for placement prior to dialysis is an important goal. Monitor for access function and complications with physical examination, dialysis findings and ultrasound monitoring.