Table of Contents
Hypertension is a prevalent issue in dialysis patients.
Mechanisms of Hypertension in ESRD patients
- Sodium and Volume Overload
- Sympathetic Overactivity
- Renin Angiotensin System Activation
Sodium and Volume Overload
The cornerstone of blood pressure control is volume management.
In non ESRD patients with hypertension (HTN), sodium/ volume overload is a reason for an inability to control BP. HTN is not classified as resistant unless the patient is treated with an adequate diuretic.
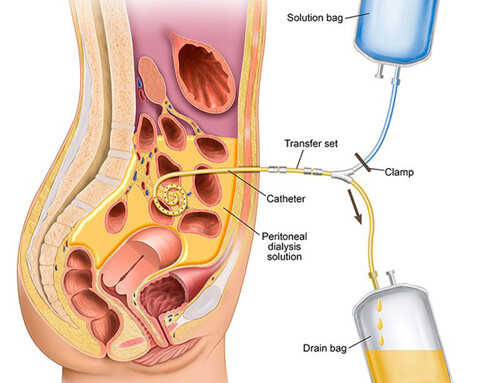
In ESRD, particularly dialysis patients who are oligoanuric, diuretics will be ineffective at achieving euvolemia.
In ESRD volume control is achieved by:
-
Sodium Restriction
- As in hypertensive patients without ESRD, dietary sodium restriction is important for dialysis patients. However, in ESRD the native kidneys and diuretics will not be sufficient to prevent sodium and volume overload. Therefore, dialysis will be the main mechanism for sodium removal from the body. For this reason the dialysate sodium concentration should be maintained < 138 meq/Liter. Higher dialysate sodium concentrations may result in a positive intradialytic sodium balance. This will result in increased thirst adversely affecting fluid restriction causing increased interdialytic weight gains.
-
Maintenance of a healthy dry weight
- Adequate ultrafiltration and achievement/ probing of a true dry weight/target weight is crucial. This becomes challenging in that ultrafiltration is often poorly tolerated with hypotension and other symptoms such as cramping. Dialysis removes fluid from the vascular space, it takes time for this fluid to equilibrate from the interstitial (edema) to the intravascular space. It takes even longer for fluid to move from third space (ascites or pleural effusion).
Dry weight reduction was studied in the DRIP trial.
Which showed that a dry weight reduction of 0.9 kg resulted in a 6.9/3.1 reduction in BP at 4 weeks.
Ultrafiltration
- The recommended maximum ultrafiltration rate is < 13 ml/ kg / hr.
- This will typically be < 1 liter/ hr. 70 kg x 13 ml/ hr = 910 ml / hr.
- Higher ultrafiltration rates are associated with higher mortality.
- When a patient has symptoms and/or hypotension with ultrafiltration during dialysis ask these 2 questions.
- Is the target weight set too low?
- Is the hourly ultrafiltration rate too high?
In many cases the answer is the latter. This will occur if there are high interdialytic weight gains. There are some patients who may not be able to tolerate even less than the maximal recommended rates of ultrafiltration.
The solution in these cases: Longer or more frequent dialysis.
The concept of longer dialysis is difficult for many patients to accept as the symptoms of cramping and hypotension often happen in the last 30 minutes of dialysis. Given this association they believe that a shorter treatment will result in avoiding the symptoms. However, this approach often backfires as the end result is a higher hourly rate of ultrafiltration, which may be less well tolerated.
Treatment of intradialytic hypotension
Algorithm for managing intradialytic hypotension:
- Assess volume status with adjustment of dry weight/target weight.
- Loop diuretics on non dialysis days for patients with residual urine output (to mitigate interdialytic weight gains).
- Avoidance of eating during dialysis to avoid postprandial splanchnic vasodilation.
- Assessment for comorbid etiologies of hypotension (ie cardiac)
- Longer or more frequent treatments
- Low temperature dialysate: Lowering the dialysate temperature by 1-2 degrees celsius may prevent vasodilation helping BP
- Ultrafiltration modeling: This is a technique where the ultrafiltration rate is not constant, but varies throughout the treatment.
- Medications
- Midodrine
- Droxidopa
- Sodium modeling. This is a technique where the dialysate sodium concentration starts high (ie 145 meq/Liter) and is gradually decreased during treatment. This has fallen out of favor and is discouraged as it results in a positive sodium balance for the patient.
Holding antihypertensives predialysis? This is commonly done, but is of unclear benefit. It is recommended to hold short acting medications (ie. hydralazine) before dialysis. I typically recommend taking once daily medications in the evening. Patients with paradoxical intradialytic hypertension may benefit from predialysis administration of beta blockers or renin angiotensin system inhibitors (see below).
Antihypertensives in ESRD
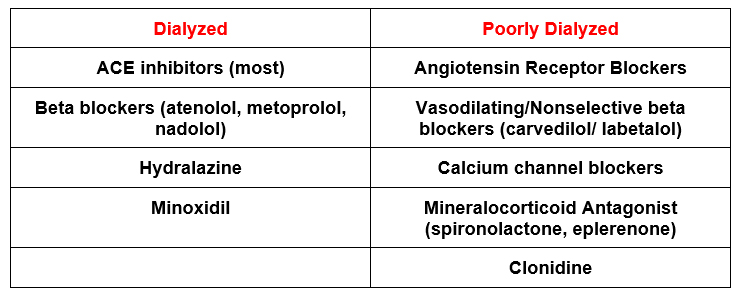
An important consideration is the potential removal of antihypertensives with dialysis. Some antihypertensives are dialyzed.
Although most patients will tend to have their blood pressure drop with ultrafiltration during dialysis, some patients may develop paradoxical intradialytic hypertension. This may be related to an increased adrenergic response to intravascular volume depletion with ultrafiltration and is associated with a worse patient prognosis.
For a comprehensive review of antihypertensives during dialysis check out this article.
The recommended stepwise approach in this article is:
- Beta blocker
- Non dihydropyridine calcium channel blocker
- Renin Angiotensin System blocker (ACEI or ARB)
- Mineralocorticoid antagonist
My approach to antihypertensives in ESRD
- Avoid medications that are dialyzable.
- Change metoprolol to carvedilol
- Change ACE to ARB
2. Avoid medications that are difficult to take (such as 3 times a day dosing) or make the patient feel like crap
- Wean off labetalol (or change to carvedilol)
- Wean off clonidine. Clonidine is particularly a concern in a patient with incomplete adherence given its association with rebound hypertension
- Wean off hydralazine
3. Add a nondihydropyridine calcium channel blocker. (ie. amlodipine, extended release nifedipine)
- These can be effective in volume overloaded states (they are used for salt sensitive hypertension in the general population)
4. Address the mechanisms of HTN in ESRD
- Sympathetic Overactivity: Carvedilol
- Renin Angiotensin System Activation: Angiotensin Receptor Blocker
5. Additional Medications:
- Mineralocorticoid receptor antagonist (spironolactone).
- These have been shown to be effective in ESRD and resistant hypertension
- Concerns about hyperkalemia, this can be typically managed with dialysis
- Minoxidil
- Potent vasodilator
- Reflex tachycardia (typically requires coadministration of beta blocker)
Summary
The management of hypertension in ESRD is difficult for the following reasons:
- There is a J curve with increased mortality associated with both high and low blood pressure. A pre dialysis systolic blood pressure < 120 is associated with greater mortality
- There is a wide variation in blood pressure with many patients having significant hypertension pre dialysis that drops during dialysis. Recommendations are:
- Target pre dialysis blood pressure < 140/90
- Target post dialysis blood pressure < 130/80
- Interdialytic home or ambulatory blood pressure measurements are better prognosticators.
Cornerstones of management of hypertension is achieving adequate sodium and sodium status with an appropriate dry weight and use of non-dialyzable medications that address sympathetic overactivity and activation of the renin angiotensin system.