Table of Contents
There are certain dermatologic conditions unique to ESRD that the nephrology practitioner should be aware of. These include:
- Uremic pruritus
- Calciphylaxis – calcific uremic arteriolopathy
- Perforating Dermatosis – Kyrle Disease
- Nephrogenic Systemic Fibrosis
Uremic Pruritus
Pruritus is a common complaint in ESRD. It may be localized or generalized.
Pathogenesis. It is often attributed to hyperphosphatemia. There are other uremic factors that contribute. Although dialysis may help (the incidence has decreased from as high as 85% to less than 50% with improved dialysis membranes and adequacy), many patients will have this symptom despite dialysis and a controlled serum phosphorus.
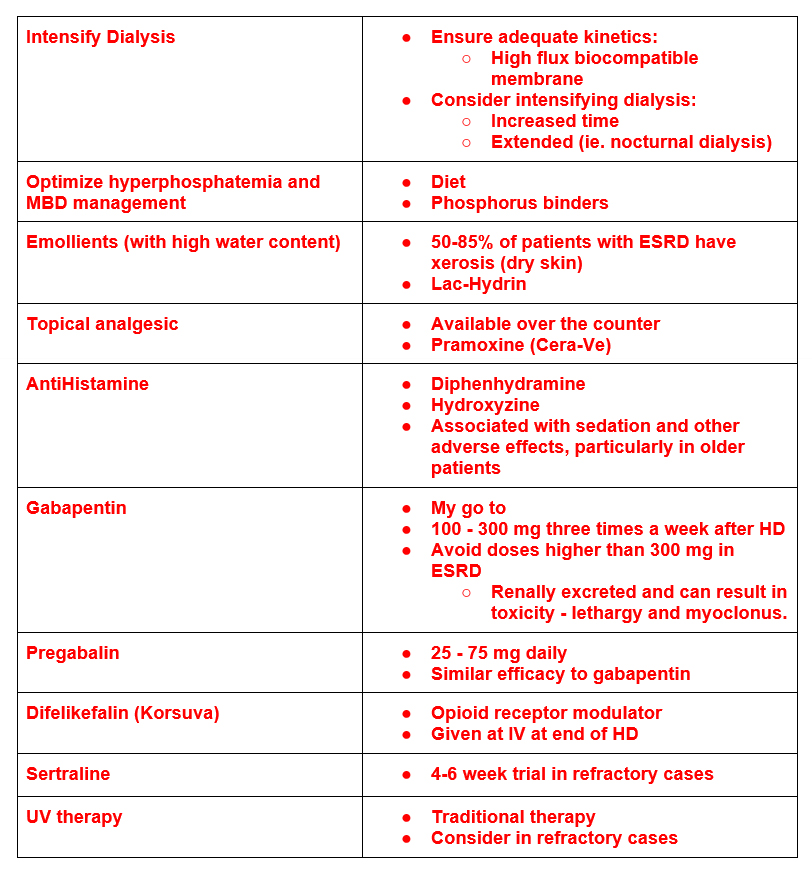
Treatment Algorithm
Calciphylaxis – Calcific Uremic Arteriolopathy
Lesions caused by calcification of the small vessels (arterioles and capillaries). The calcification leads to obstruction of these vessels resulting in painful infarction of the tissues. Occurs in areas where body fat is prominent such at the abdomen, buttocks, lateral posterior leg.
Risk Factors:
- Trauma sites ( ie insulin injection sites)
- Diabetes
- Warfarin
Presentation:
- Painful skin lesions
- Livedo reticularis ➞ plaques or nodules ➞ ulcerations
- Ulcerations may be secondarily infected.
Differential Diagnoses:
- Warfarin skin necrosis
- Venous stasis ulcer
Diagnosis:
- Biopsy: Calcification of medial layer and internal elastic membrane
- Proceed with caution – biopsy provide trauma nidus for ulceration
- Imaging:
- Bone scan: Calcified areas in dermis/ subcutaneous fat
- X Ray: Vascular calcification
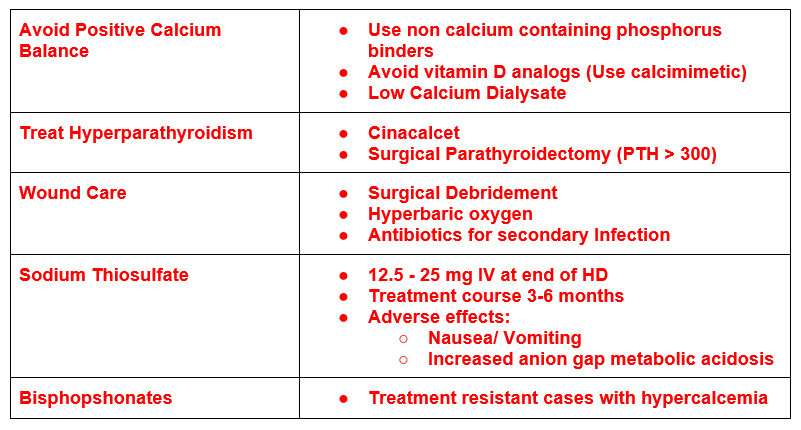
Treatment:
Overview of Mineral Bone Disease Treatment Dialysis Rounding Primer – Mineral Bone Disease (CKD-MBD) | BCNephro
Kyrle disease- Perforating dermatoses
Presentation:
- Pruritic dome shaped papules with central keratin plug (white or yellowish color)
- Location: extensor surfaces of extremities and trunk
- Risk factors:
- African Americans
- Diabetes
Treatment:
- Antihistamines (oral)
- Topical antipruritic agents (ie camphor)
- Topical corticosteroids
- Topical salicylic acid
- UV phototherapy
Nephrogenic Systemic Fibrosis
This is a skin condition that was a complication of gadolinium in ESRD patients. It had been common for patients with ESRD to have magnetic resonance angiography (MRA) as opposed to CT angiography (CTA) to avoid the nephrotoxicity of CT contrast. Gadolinium is not nephrotoxic, but was associated with the complication of nephrogenic systemic fibrosis.
Pathogenesis:
- Gadolinium is renally excreted. Half life increases from 1-2 hrs – 60 hours in ESRD
- Over time gadolinium dissociates from its chelate into its ionic form
- Ionic form of gadolinium can bind with phosphates and is toxic to tissues (can stimulate fibrogenesis)
Clinical Manifestations:
- Hyperpigmentation/ plaques ➞ skin thickening (scleroderma like) ➞ joint contractures
- Progressive, debilitating and painful.
- Associated with high mortality.
Fortunately this has become less common, as a nonlinear form of gadolinium (Type II agent) was developed. These newer formulations are not associated with NSF. These have become the main gadolinium agents and should be used in all patients with advanced CKD (eGFR < 30) or ESRD. As gadolinium is dialyzable, it is often suggested to coordinate dialysis after its administration. This is reasonable if it can be coordinated, but not absolutely necessary given the low risk of NSF with the Type II gadolinium agents.
Summary:
There are dermatologic conditions that are unique to advanced CKD/ ESRD. These include:
- Uremic pruritus
- Calciphylaxis – calcific uremic arteriolopathy
- Perforating Dermatosis – Kyrle Disease
- Nephrogenic Systemic Fibrosis
It is useful to be aware of these conditions and their management when caring for dialysis patients.
For additional information check out this article: https://journals.lww.com/cjasn/pages/articleviewer.aspx?year=2014&issue=01000&article=00027&type=Fulltext



