Table of Contents
So some people don’t think contrast nephropathy is real (Don’t look up).
The American College of Radiology and National Kidney Foundation looked at the data:
Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation
It is also reviewed in the American College of Radiology Manual on Contrast Media:
ACR Manual On Contrast Media
**This is for intravenous contrast, the risk for AKI after arterial contrast (ie for an catheterization) tends to be higher.
We know this, some people get acute kidney injury (AKI) after they receive contrast. The argument is that they would have gotten AKI anyway. These are patients who tend to be sick with a lot of things going on. Sick patients are at risk for AKI.
To differentiate this new terminology was created:
Contrast Associated Acute Kidney Injury (CA-AKI): AKI that occurs after IV contrast.
Contrast Induced Acute Kidney Injury (CI-AKI): AKI that occurs because of contrast.
To figure this out they looked for studies with a control group. The assumption being that the difference in AKI incidence in the group that received IV contrast (CA- AKI) and the matched control group that didn’t get contrast would be the expected incidence of AKI that was caused by contrast. That is contrast induced AKI ( CI-AKI).
Studies like this are flawed in general, but they’re not going to randomize people to contrast or no contrast and blind them by giving sham contrast. So that’s the best we have.
Here’s what they found. The main risk factor for contrast nephropathy is CKD. The table below shows the incidence of contrast associated (CA) and contrast induced (CI) AKI based on the studies.
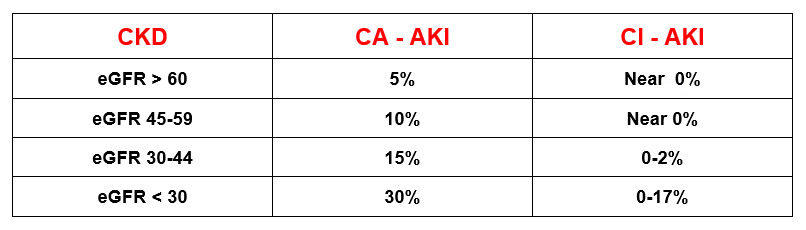
Bottom line is this, maybe contrast doesn’t statistically cause AKI (unless CKD with eGFR < 30) because many would have gotten AKI anyway, but getting kidney failure sucks.
Personal opinion. I wouldn’t be cavalier about doing something that might cause AKI.
My Approach to Assessing Risk for Contrast Nephropathy
- Everything in medicine is a risk benefit ratio. The risk is either high, low, or theoretically possible. The benefit is either high, low, or theoretically possible.
The ACR Manual On Contrast Media says this:
“In fact, since each contrast medium administration always implies a risk-benefit analysis for the patient, contrast medium administration for all patients should always be taken in the clinical context, considering all risks, benefits and alternatives”
So:
- If the benefit of contrast is extremely high, it may make sense to give the contrast even with CKD 4 or 5 (eGFR < 30) or AKI (see below).
- If the benefit of contrast is very low, it may make sense to not give contrast for lesser degrees of CKD (ie. CKD stage 3).
- The risk assessment is for CKD not AKI. In AKI the eGFR does not accurately reflect the true level of kidney function because it is based on the creatinine (which lags behind the true eGFR).
Bottom line if the creatinine is not stable the eGFR is not accurate.
The ACR Manual On Contrast Media says this:
“patients with AKI are particularly susceptible to nephrotoxin exposure and therefore it is probably prudent to avoid intravascular iodinated contrast medium in these patients when possible.”
- My additional approach is this. An additional caution eGFR range (30-44)
For patients with an eGFR 30-44 (consistent with CKD 3b) there is a hard pause to ask the following questions:
- Am I sure that this is not acute kidney injury?
- Are there other risk factors for contrast nephropathy?
- Is contrast absolutely necessary or is alternative imaging acceptable?
At this eGFR it is the physician’s responsibility to rule out AKI. This would require knowing or obtaining the baseline creatinine/ eGFR. If this is not available one must work from the possibility that this is AKI and not CKD. The risk benefit ratio of administering contrast then should be weighed in this context.
If the eGFR is > 45 then the possibility of AKI being present is less likely and if it is it is likely to be less severe. In these cases the risk of contrast would be much less.
How to not make it happen
If contrast isn’t given CA or CI AKI can’t happen. So we have reviewed the 1st way to not make it happen. Assess the risk and if possible avoid its administration in high risk patients.
The guidelines recommend discussion between the radiologist and referring physician for patients with AKI, eGFR < 30, and dialysis patients that are non anuric (residual urine output >100 ml day)
The other way to mitigate the risk is to give prophylactic IVF. The fluids should be Normal Saline (0.9%).
If you look at the document (ACR Manual On Contrast Media) it recommends prophylaxis with NS for:
- Patients with AKI.
- CKD with eGFR < 30 (not dialysis).
- Individual high risk cases with eGFR 30-44 at the discretion of the physician (borderline GFR, recent AKI, numerous risk factors for AKI) being the considerations
Summary
We should not be using a single eGFR cutoff to decide if it’s “okay” to give IV contrast or not. It should always be a risk-benefit decision.
I agree with the American College of Radiology Guidelines that
- There should be a discussion between the ordering physician and radiologist if the eGFR is < 30.
In addition I propose that
- There is an “internal dialog” if the eGFR is 30-44 to ask, Am I sure that this is not acute kidney injury? Are there other risk factors for contrast nephropathy? Is contrast absolutely necessary or is alternative imaging acceptable?



