Table of Contents
Continuous Renal Replacement Therapy (CRRT). Slow dialysis for critically ill hemodynamically unstable patients. The main benefit of CRRT is that it is better at treating and preventing volume overload in these patients.
The main benefit of CRRT. Volume management. It allows for ultrafiltration at a slower rate. How do we decide on ultrafiltration in our hemodynamically unstable patient? There are 3 models.
Net Ultrafiltration:
This is the traditional method:
How it’s Done:
- Nephrologist prescribes a Net hourly ultrafiltration (UF) rate. Observational studies have observed the lowest mortality with Net negative UF rates of 1.0 – 1.75 ml/hg/hr. Association of Net Ultrafiltration Rate With Mortality Among Critically Ill Adults With Acute Kidney Injury Receiving Continuous Venovenous Hemodiafiltration: A Secondary Analysis of the Randomized Evaluation of Normal vs Augmented Level (RENAL) of Renal Replacement Therapy Trial | Critical Care Medicine | JAMA Network Open
- Nurse calculates the hourly required UF rate (calculates previous hour input/output balance and adds prescribed UF) and adjusts CRRT machine hourly.
- Example:
- Prior hour input (drips/medications) 150 ml – Prior hour output (drains/urine/GI) 50 ml = 100 ml
- Prescription (Net UF negative 75 ml/hr)
- 100 ml + 75 ml = 175 ml
- Set Machine UF 175 ml for subsequent hour.
- Example:
Pitfalls:
On face value this seems a logical approach. It certainly is the easiest for the nephrologist to order. However, there are some real life practical downsides.
- More labor intensive for nurse
- Wide fluctuations in actual hourly ultrafiltration. Example: Order net UF order 100 ml/ hr.
- Hour 1: Ins: 100 ml in drips + net UF 100 ml: Machine UF set 200 ml for subsequent hour
- Hour 2: Ins: 100 ml drips + 300 ml in antibiotics + net UF 100 ml: Machine UF set 500 ml for subsequent hour
In many cases the higher UF cannot be achieved. An inability to tolerate higher UF rates is why they are on CRRT in the first place. The result:
- Either play catch up in subsequent hours or
- The patient doesn’t achieve the intended daily negative fluid balance.
- Not adaptive for the most hemodynamically unstable patient. Doesn’t allow for positive fluid balance. Examples:
- Patient requires a fluid bolus. Based on the order does the nurse remove the bolused volume? Of course not, that doesn’t make sense.
- CRRT is for metabolic reasons (hyperkalemia and/or acidosis) and is too unstable for any UF. The intention is for a positive fluid balance. The order is UF 0. However, based on this model 0 UF is interpreted as Net 0. Fluid would still be removed (based on input) to keep the patient even.
Perspective: This degree of micromanaging is not necessary. If you want the patient a liter negative for the day do they have to be exactly 42 ml negative every hour? Or is a liter negative for the day ok? Do they have to be exactly 1 liter negative? Or is 750 ml or 1250 ml negative ok?
I am an advocate of the following models:
Fixed Ultrafiltration Rate: Target 24 hour balance
How it’s Done:
- Step 1: Add up all the hourly rate of drips. Example: Drips 75 ml/hr x 24 hrs = 1800 ml/ day.
- Step 2: Estimate volume of prescribed meds for the day. Just talk to the nurse. If unsure 500 ml/day is often a reasonable estimate. Example: Volume of antibiotics, riders, meds = 500 ml/ day.
- Step 3: Decide target fluid balance. Just talk to the critical care team. Example: Goal fluid balance: Negative 1 liter for the day.
- Step 4: Add them up and divide by 24. Example: 1800+500+1000 = 3300 day = 137.5 ml/hr. Can round up a bit to account for unanticipated medications/ machine down time. Rx: UF rate 150 ml/ hr
Pitfalls:
But what if things change? That’s the counter argument. You prescribe a UF rate that will achieve the target 24 hour fluid balance. Something changes (i.e. the patient needs transfusions or additional medications). The target fluid balance isn’t achieved.
Safeguards:
- Sliding Scale UF titration:
- Step 1: Decide target fluid balance and acceptable target range: Example: Target 24 hour fluid balance negative 1.5 liters, acceptable range negative 1- 2 liters.L.
- Step 2: Periodically assess if on track to achieve target fluid balance (i.e. every 6 hrs) and course correct as needed. Example for target fluid balance negative 1-2 liters L: If not negative by greater than:
- 250 ml at 6 hrs
- 500 ml at 12 hrs
- 750 ml at 18 hrs
- Then increase set UF rate by 50/hr
- If negative greater than target 24 hour target balance then decrease set hourly UF.
- Protocolize maximum allowable UF rate.
- We require nephrology approval for hourly UF rates > 300 ml/ hour.
- If worsening hemodynamic status (increased pressor requirement, worse MAP) contact critical care service for reassessment. In this case a decision can be made (in consultation with the nephrologist) to either:
- Decrease the hourly UF rate.
- Prescribe a fluid bolus or
- Continue current UF rate with uptitration of vasopressors.
A better way would be to develop a calculator in the EMR and/or dialysis machine. A program where the nurse enters the ins and outs and the target fluid balance. The program calculates the set hourly UF rate for the remainder of the day. If this calculator could be automated it could course correct on the fly.
Fixed Ultrafiltration Rate: Titration as hemodynamically tolerated:
This is for the most critically unstable patient. So unstable that it’s not clear that any fluid removal is possible. The patient will require a positive fluid balance.
How it’s Done:
- Set the initial UF rate to 0. No fluid removed. Patient is positive. CRRT is for metabolic indications (acidosis, hyperkalemia).
- If hemodynamically stable (i.e. stable or decreased pressor requirement, stable or increased MAP) then uptitrate hourly UF rate. Example by 50 ml/ hr every 6 hrs with a maximum UF rate not to be exceeded. The patient may still be positive, but this will mitigate the positive balance.
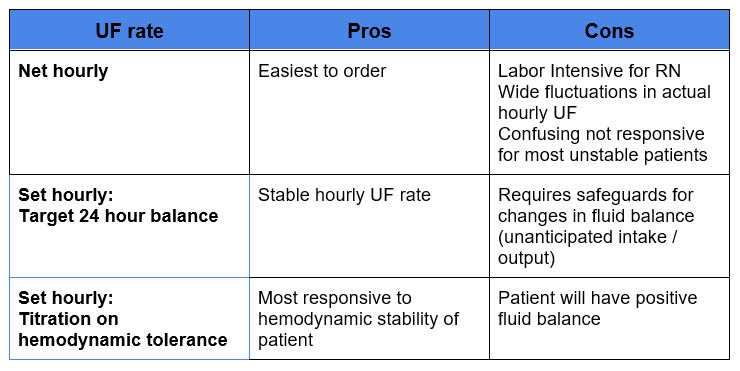
Summary:
The main benefit of CRRT is volume management. This is achieved by the ultrafiltration strategy. The traditional strategy of Net hourly ultrafiltration can lead to wide fluctuations in actual hourly ultrafiltration. A Set hourly ultrafiltration rate if protocolized well may be an effective strategy.
Let me know your thoughts about the best strategy in the comments below.