Table of Contents
This article will provide a framework for evaluation of the patient with abnormal kidney function (elevated serum creatinine/ decreased estimated Glomerular Filtration Rate (eGFR).
When evaluating a patient with Chronic Kidney Disease (CKD), I have the following considerations:
- Is there something bad?
- Is it chronic?
- What is the underlying cause?
Is There Something Bad?
This typically would be a complication of CKD that is severe enough to warrant urgent treatment and/or dialysis.
- Uremia
- Hyperkalemia
- Metabolic acidosis
- Volume Overload
This should be readily apparent on the available laboratory studies (metabolic panel) and/or physical examination.
Is it Chronic?
The definition of Chronic Kidney Disease (CKD) is kidney damage (such as increased serum creatinine/ decreased eGFR) for > 3 months. This needs to be distinguished from Acute Kidney Injury and Subacute Kidney Injury/Acute Kidney Disease.
Acute Kidney Injury (AKI) is worsening of kidney function (increase in creatinine by > 0.3mg/dl or by > 50% from baseline) over hours to days.
Subacute Kidney Injury (Acute Kidney Disease) is worsening of kidney function over > 48 hrs to < 3 months.
In AKI or Acute Kidney Disease, the underlying etiology would need to be diagnosed to prevent potential life threatening complications and/or irreversible kidney damage.
Often in the outpatient/ambulatory setting there are transient increases in creatinine related to illnesses or medications. This most often would be Subacute Kidney Injury (Acute Kidney Disease).
The way to differentiate Chronic Kidney Disease (CKD) from Acute Kidney Injury/Disease is to compare the current kidney function (creatinine/ eGFR) to prior values.
- Current kidney function (Creatinine/ eGFR) similar to prior kidney function: CKD – Evaluation as below. (link to) What is the underlying cause of the CKD – section below
- Current kidney function (Creatinine/ eGFR) significantly worse (creatinine increased by >0.3 g/dl or 50%) from prior kidney function: AKI/AKD.
- Triage for emergent treatment (oliguria, rapidly rising creatinine, life threatening complications)
- Prompt evaluation for reversible causes:
- Prerenal
- Medications
- Acute Interstitial Nephritis
- Glomerulonephritis
- Postrenal/obstructive uropathy
- No prior kidney function available:
- Review for acute dehydrating illness or urinary obstruction symptoms
- Review for medications that may affect kidney function and hold if possible.
- NSAIDS
- RAS Blockers (Angiotensin Receptor Blockers/ ACE inhibitors)
- Diuretics
- Antibiotics (ie. TMP-SMX)
- Fibrates
- Assess for signs and symptoms suggestive of AKI (oliguria, uremia)
- Timely reassessment of kidney function (within 1-2 weeks)
What is the Underlying Cause of the CKD
CKD is a clinical syndrome, not a specific diagnosis. In all cases a specific diagnosis should be sought. This specific diagnosis may be:
- Biopsy proven
- Presumed
- Not known. I refer to this as CKD of unclear etiology.
As in AKI the differential diagnosis for CKD includes:
- Prerenal (Chronic prerenal states)
- Heart failure/ Cirrhosis
- Medications (Diuretics; RAS blockers; NSAIDS)
- Intrinsic Renal
- Glomerular (glomerulonephritis/ glomerulopathy)
- Tubulointerstitial (Nephrosclerosis; interstitial nephritis; prior AKI/ATN with incomplete recovery; medication toxicity – lithium, chemotherapy)
- Obstructive/Post Renal
- Chronic obstructive uropathy may result in irreversible kidney damage.
Medications Associated with CKD
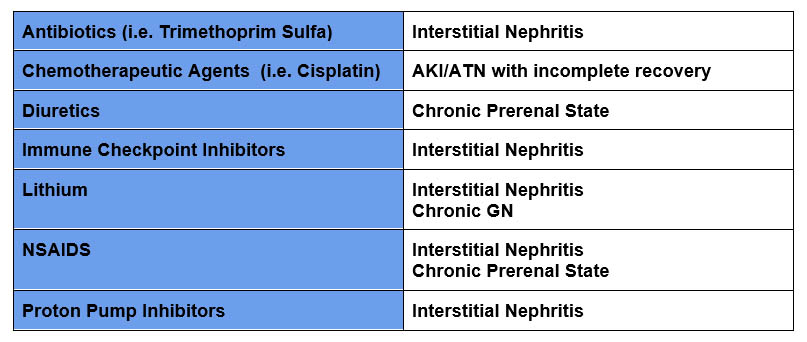
The above is not a comprehensive list, but some of the more common medication causes I have encountered.
Framework for Evaluation of CKD
Here is my framework. I consider CKD in the context of:
- Systemic diseases
- Presence or absence of proteinuria
- Structural kidney abnormality.
The above framework informs the evaluation.
Systemic diseases Associated with CKD
These include:
- HTN
- Diabetes
- Malignancy
- CV disease
- Rheumatologic disease
Sometimes the systemic disease will be apparent, sometimes kidney disease will be the presenting finding leading to its diagnoses. Physical and laboratory evaluation should look for findings suggestive of systemic conditions such as:
- Cardiovascular: Bruits, signs of heart failure
- Skin: Rashes, palpable purpura, livedo reticularis
- Laboratory: Anemia; thrombocytopenia; hypercalcemia
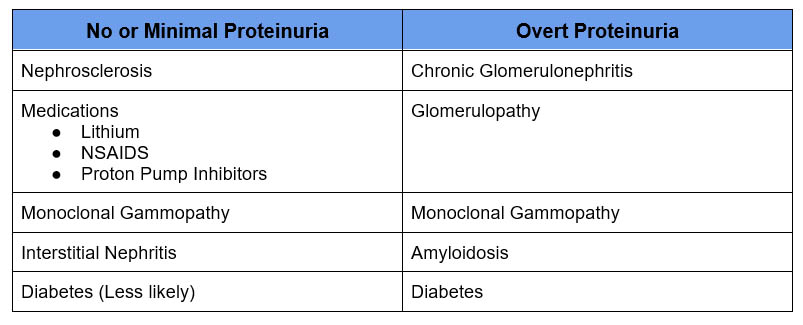
Presence or absence of proteinuria
I check the following as part of my evaluation:
- Urinalysis
- Urine Albumin Creatinine Ratio (UACR)
- Urine Protein Creatinine Ratio (UPCR)
Urinalysis:
- Proteinuria: The UA gives a ballback idea of the degree of proteinuria. It can underestimate or overestimate based on the specific gravity and urine pH.
- Dilute urine – low specific gravity may underestimate the degree of proteinuria.
- Concentrated urine – high specific gravity may overestimate the degree of proteinuria
- Alkaline urine pH >0 may result in a false positive urine protein on the UA dipstick
- The urinalysis tests for albumin not for non albumin protein will not detect
- Tubular proteinuria (Interstitial nephritis)
- Overflow proteinuria (Bence-Jones, Monoclonal gammopathy)
- Hematuria: If hematuria is present need to consider a glomerulonephritis link – Glomerulonephritis: Hematuria and the Nephritic Syndrome | BCNephro
- Leukocyturia: In the absence of a urinary infection, WBC on UA may suggest an interstitial nephritis of glomerulonephritis.
For my initial assessment I typically check both a urine albumin creatinine ratio and protein creatinine ratio. Link – Proteinuria: What is it and How I Treat | BCNephro
- For glomerular proteinuria the urine albumin creatinine ratio is @ 55-60% of the protein creatinine ratio.
- If this is much lower consider:
- Tubular proteinuria (interstitial nephritis)
- Overflow proteinuria (monoclonal gammopathy)
Structural Renal Abnormality
Renal Imaging should be performed in all cases. Most often this will be with an ultrasound. It may be CT of the abdomen and pelvis (without IV contrast).
What am I looking for on imaging?
- Obstructive uropathy
- Chronic bladder outlet obstruction
- Malignant obstruction
- Obstructing Nephrolithiasis
- Congenital Kidney Disease (CAKUT)
- Cystic dysplasia
- Renal atrophy
- Vesicoureteral reflux
- Cystic Kidney Disease
- Autosomal Dominant Polycystic Kidney Disease (ADPKD) Approach to Evaluation of Renal Cysts | BCNephro
- Renal atrophy
- Bilateral suggests chronicity
- Unilateral may suggest renovascular disease
- Echogenicity
- Increased renal echogenicity suggests CKD (renal scarring)
Summary
The approach to evaluating patients with chronic kidney disease includes:
- Triage for urgent complications
- Differentiation from Acute Kidney Injury, Acute Kidney Disease
- Assessment of Cause
- Systemic Conditions
- Presence or absence of proteinuria
- Assessment of structural kidney abnormality.



