Table of Contents
ANCA associated Glomerulonephritis is the most common Rapidly Progressive Glomerulonephritis (RPGN) and it occurs in older patients.
What is ANCA Associated Vasculitis?
ANCA associated vasculitis is a small vessel vasculitis. It is an idiopathic autoimmune condition that manifests as necrotizing inflammation of small vessels with little/no immune complex deposition. As there is little or no immune complex deposition associated it is also referred to as pauci-immune.
In the kidneys it presents as a Necrotizing Crescentic Glomerulonephritis (NCGN).
90% of cases will be ANCA positive in the serum, 10% will be ANCA negative. There are two main types of ANCA.
- Cytoplasmic: C-ANCA. This is associated with Proteinase 3 (PR3)
- Perinuclear: P-ANCA. This is associated with Myeloperoxidase (MPO)
How Does ANCA Associated Vasculitis Present?
ANCA associated vasculitis can be renal limited or systemic.
Renal Manifestations:
The classic renal manifestation is a Rapidly Progressive Glomerulonephritis (RPGN).
- A rapid decrease in kidney function (increase in creatinine/ decrease in eGFR) over weeks to months.
- Glomerular hematuria (dysmorphic red blood cells and/or red blood cell casts).
- White blood cells on urinalysis without evidence of infection.
- Typically moderate (non nephrotic range, i.e. 1-3 grams/gram).
Systemic Manifestations:
- Pulmonary: Pulmonary hemorrhage; lung nodules/ cavitary lesions; hemoptysis; cough; dyspnea
- Neurologic: Mononeuritis multiplex (i.e. foot drop): peripheral neuropathy
- GI: Abdominal pain; Bleeding
- ENT: Sinusitis; saddle nose deformity
- Skin: Palpable purpura, livedo reticularis; ulcerations
- Musculoskeletal: Arthralgias; myalgias
Tip: Be aware of a smoldering presentation. ANCA vasculitis may present with nonspecific constitutional symptoms (weight loss, fever). I have seen cases of ANCA associated RPGN that in retrospect had chronic pulmonary symptoms (such as cough that was attributed to bronchiectasis) or chronic sinusitis and subsequently developed an accelerated decline in kidney function.
There are 3 different clinical syndromes.
- GPA – Granulomatosis with Polyangiitis: associated with C-ANCA/PR3 antibody
- Less common
- ENT – involvement more common
- Renal and lung involvement common
- MPA – Microscopic Polyangiitis: associated with P-ANCA/ MPO antibody.
- More common: Age > 50, men > Women
- More likely to be renal limited
- Lung involvement common
- e-GPA – Eosinophilic Granulomatosis with Polyangiitis: associated with P-ANCA/ MPO antibody
- Less common
- Renal involvement less common
- Asthma common
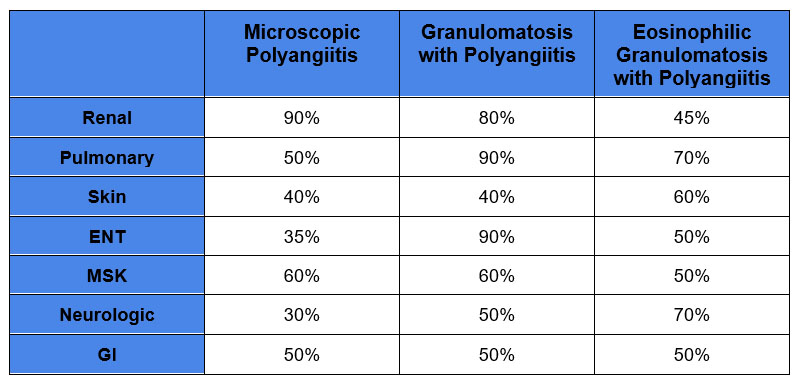
Organ Involvement in ANCA Associated Vasculitis
Drug induced ANCA Vasculitis
- Hydralazine
- TNF inhibitors (Infliximab; etanercept; adalimumab
- Propylthiouracil
Tip: A clue to drug induced ANCA vasculitis is positivity to multiple antibodies (i.e. positive for ANCA and ANA and/or positive for both P and C ANCA)
How to Diagnose ANCA Associated Vasculitis
Clinical Presentation:
This diagnosis is considered when there is an acute/subacute decline in kidney function, especially if associated with pulmonary hemorrhage or other signs of systemic vasculitis.
There will be an abnormal urinalysis with
- Glomerular hematuria (dysmorphic RBC)
- Proteinuria
- +/- Leukocyturia
Can’t depend on the lab (either as inpatient or outpatient) to report dysmorphic RBC’s or RBC casts. If nephrology consult (either inpatient or outpatient) the urine microscopic specimen can personally be examined for these elements.
If there is hematuria, but the presence of dysmorphic RBCs cannot be established, consider the clinical context.. Can the hematuria/leukocyturia be explained by another etiology such as urinary infection or catheter? Is there associated proteinuria? If there is no explanation for the hematuria/leukocyturia and there is proteinuria need to consider glomerulonephritis.
At this point ANCA vasculitis may be suspected, but there is a differential which includes:
- Anti Glomerular Basement Membrane (GBM) antibody disease (Goodpasture’s)
- Immune Complex Glomerulonephritis
Serologies
- ANCA panel, Myeloperoxidase Antibody, Proteinase 3 antibody
- Anti glomerular basement membrane antibody. Important to check as there may be dual positive ANCA/GBM RPGN. The presence of both antibodies has implications for treatment.
- Complements C3 and C4 (Often low in immune complex GN)
The above serologies (with the exception of complements) are often send out tests with a delayed turnaround time for results. If the is high suspicion need to proceed with:
Kidney biopsy
Pauci-Immune Focal and Segmental Necrotizing Crescentic GN
- Light microscopy will show a proliferative necrotizing crescentic glomerulonephritis. However this does not distinguish ANCA associated GN from anti GBM antibody or immune complex GN. If you are fortunate to see the following you may
- Granulomas – suggest granulomatosis with polyangiitis
- Necrotizing inflammation of a small vessel.
- This is where the money is at
- Negative immunofluorescence points toward ANCA associated GN
- Linear staining suggests anti GBM antibody disease
- Granular staining suggest immune complex GN
Treatment of ANCA Associated Glomerulonephritis
ANCA associated vasculitis is a relapsing condition. Therefore treatment is split into:
- Induction
- Maintenance
Induction
Consists of steroids plus immunosuppression +/- plasmapheresis
Steroids:
- Pulse steroids: Methylprednisolone 1 gram IV daily x 3 days
- Oral steroids: Prednisone. An accelerated Prednisone taper found to be as effective as the traditional slower steroid taper in the PEXIVAS study. Plasma Exchange and Glucocorticoids in Severe ANCA-Associated Vasculitis – PMC
To see the accelerated prednisone taper schedule check out page 21 here:
https://www.nejm.org/doi/suppl/10.1056/NEJMoa1803537/suppl_file/nejmoa1803537_protocol.pdf
Avacopan: C5a receptor antagonist. This is a newer drug that can limit steroid doses. Personally, at the time of writing this article I have not used it yet.
Immunosuppression: Consists of either
- Rituximab
- Often used as it is considered safer. This is certainly reasonable in older or frail patients.
- Given as 1 gram x 2 separated by 2 weeks
- Cyclophosphamide
- Younger non frail patients, especially if they have severe renal failure.
- If concomitant GBM antibody positivity
- Can be given in IV pulses or oral
- IV 15 mg/kg every 2 weeks x 3 doses then every 3 weeks for 3-6 months
- Oral 1.5-2.0 mg/kg daily for 2-6 months.
IV pulses are often recommended (with IV there is a lower total cumulative dose), but I prefer oral. If used for only for 3-6 months the cumulative dose is not excessive.
Plasmapheresis: Indicated if
- Severe renal failure. (i.e. dialysis requiring or severe creatinine increase >5.7 mg/dl)
- If associated pulmonary hemorrhage
- If concomitant GBM antibody positivity
Maintenance: For 18-24 months
- Azathioprine: Traditionally given after cyclophosphamide induction
- Rituximab: Can be given at months 6,12,18 after induction with either Rituximab or cyclophosphamide.
A dilemma is how long to continue maintenance therapy in a patient with dialysis dependent kidney failure. I believe that if there are no extrarenal/systemic vasculitis manifestations immunosuppression should be limited to 3- 6 months. After this risks outweigh benefits as renal recovery is unlikely. This may require close communication with other specialists to establish the presence or absence of systemic disease to avoid the “You’re treating the kidneys anyway” mentality.
Summary
ANCA associated glomerulonephritis is an important consideration especially in older patients who present with a rapid decline in kidney function with an active urine sediment. There may be associated manifestations of systemic vasculitis. Be mindful that this condition can have a smoldering course with constitutional or nonspecific pulmonary or ENT symptoms. Consider it as a cause of drug induced vasculitis, especially with hydralazine.



