Table of Contents
Interstitial Nephritis is an important cause of Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD). This article will talk about Acute Interstitial nephritis (AIN)
- AIN may be difficult to diagnose.
- AIN is relatively common. 1 study found that 12.9% of renal biopsies for AKI showed interstitial nephritis.
- AIN may cause severe AKI with oliguria and requiring renal replacement therapy.
- AIN had evolved. The classical triad of fever, rash, and eosinophilia that was observed with methicillin induced AIN is rare today.
- Proton pump inhibitors and Immune checkpoint inhibitors have become more common causes of AIN.
This article will discuss:
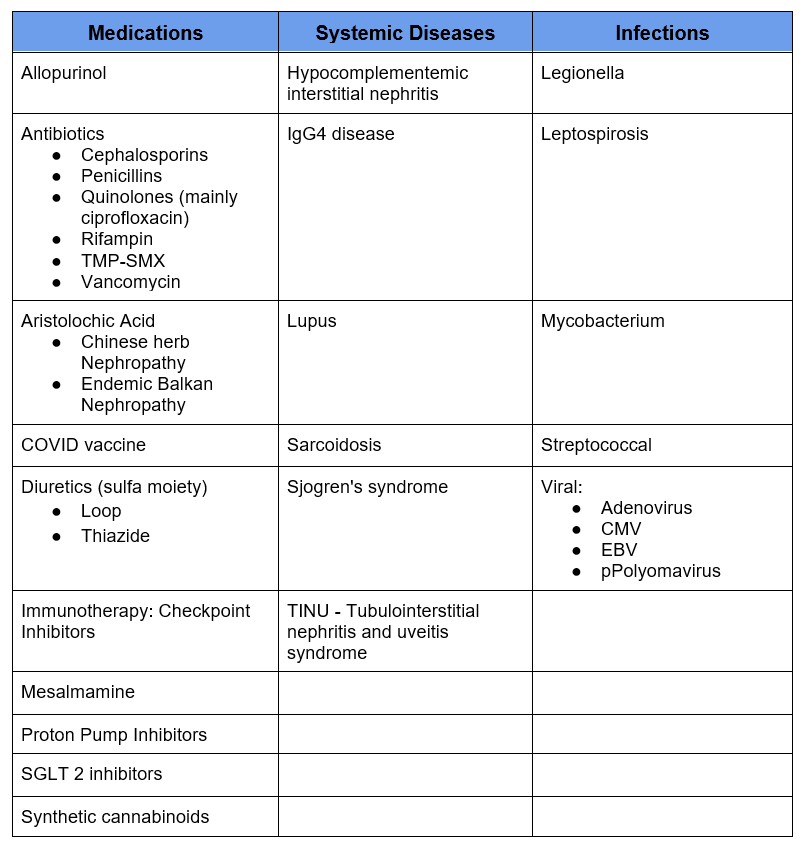
- Causes of AIN
- Diagnosis of AIN
- Treatment of AIN
Causes of AIN
AIN is most commonly attributed to medications. However, there is a broader definition including systemic diseases and infections.
Medication Causes of AIN: Pearls
- Proton Pump Inhibitors
- May be associated with chronic kidney disease
- Interstitial Nephritis is rare side effect of PPIs, however given their common use it has become one of the more common causes of Acute Interstitial Nephritis
- Immune Checkpoint Inhibitors
- More common with CTLA4 inhibitors (ipilimumab) alone or in combination with PD1 inhibitors
- 69% on other medication associated with AIN (such as PPI’s)
- Median presentation 14 weeks (interquartile 6-37 weeks)
- Antibiotics
- PCN/ cephalosporins are most commonly considered
- Consider other antibiotics especially: Quinolones (mainly ciprofloxacin); Rifampin; TMP-SMX; Vancomycin
- NSAIDS/ COX 2 inhibitors
- Nephrotic proteinuria: unique AIN presentation
- Minimal change disease on renal biopsy
- Allopurinol
- DRESS syndrome: Drug Reaction with Eosinophilia and Systemic Symptoms
- Many consider allopurinol nephrotoxic. In the absence of AIN I consider it to be safe in CKD although there may be higher incidence of rash. Start at lower doses.
- Aristolochic Acid.
- More often causes CKD
- Implicated in both:
- Balkan Endemic Nephropathy
- Chinese herb Nephropathy: Described in certain herbal/ weight loss preparations
Systemic Diseases Associated with AIN
Rheumatologic conditions can be associated with glomerulonephritis or interstitial nephritis. The following are more likely to present with interstitial nephritis
- Sjogren’s syndrome
- More often chronic, may be subacute
- Sjogren’s may also be associated with:
- Renal Tubular Acidosis (RTA)
- Fanconi’s syndrome
- Membranoproliferative glomerulonephritis (MPGN)
- Sarcoidosis
- 20% of patients with sarcoidosis may have, but often subclinical (preserved GFR)
- Granulomatous Interstitial nephritis
- Typically presents at time of initial diagnoses
- IgG4 disease:
- Associated findings include pancreatitis, cholangitis, salivary gland enlargement, lymphadenopathy and retroperitoneal fibrosis
- Measure IgG subclass: Many will have elevated IgG4 level
- Biopsy confirmation
- TINU: Tubulointerstitial nephritis and uveitis syndrome
- May cause AKI
- Clue of eye symptoms (eye pain and/or redness)
Infectious Causes of AIN
- Many infections have been associated with Acute Interstitial Nephritis. See table.
- Consider as cause of AKI with viral infections
Diagnosis of AIN
AIN may cause AKI , but there is no finding to hang your hat on, besides for renal biopsy.
Here is my approach – things I consider. Clinical Findings and When to perform RenaL Biopsy
Clinical Findings
- Clinical Presentation
- On a medication that is known to cause AIN?
- Is the timing of the medication coincident with the development of AKI?
- Days – Weeks (antibiotics)
- Weeks – Months (PPIs; Immunotherapy)
- Clinical Clues. Are any of the following present?
- Fever
- Rash
- Eosinophilia
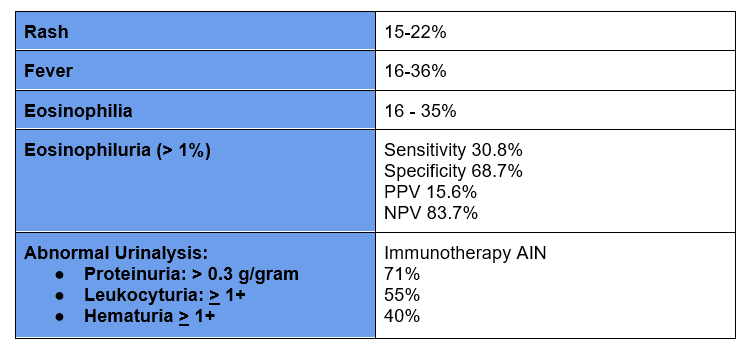
- Abnormal urinalysis
- Leukocyturia
- Hematuria – usually microscopic
- Proteinuria – usually subnephrotic (exception NSAIDS)
- Urinary eosinophils: Utility of Urine Eosinophils in the Diagnosis of Acute Interstitial Nephritis – PMC
- Is there another likely cause of AKI?
- Rule out prerenal, acute tubular necrosis, glomerulonephritis
Prevalence of Clinical Findings
When to Perform Renal Biopsy
I consider renal biopsy in the following situations:
- When there is a compelling indication to continue the suspected culprit medication
- Immunotherapy
- Certain antibiotics for severe infections (i.e endocarditis)
- When there is a broad differential of potential causes of AKI
- Some medications can or associated illness can cause ATN or GN
- If findings (such as active urine sediment) suggest another possible cause
- When AIN is suspected in severe, progressive AKI
- When I am considering treatment with steroids.
Treatment of AIN
- Stop Culprit medication
- Steroids: Although data is conflicting most would advocate use of steroids in the following situations:
- Severe AIN (especially if biopsy proven)
- Failure of improvement in AKI after holding medication for 3-7 days
- Steroids are more effective if started within 7 days
- Steroid Regimens
- Pulse methylprednisolone x 3 days. Recommended by some for severe AKI such as that require or may imminently require dialysis.
- Prednisone
- 5 mg/ kg x 4 weeks, taper x 4 weeks or
- 1 mg/ kg x 2 weeks followed by taper.
The regimen I would use is 1 mg/kg (I typically use 60 mg day) x 2 weeks with subsequent taper
- Checkpoint inhibitor rechallenge. If the regimen has had an antineoplastic effect I make every effort to allow resumption. The following may facilitate.
- Stop other culprit medications. Many are concomitantly on PPIs which can be weaned.
- If combination CTLA4/PD1 regimen consider using PD1 alone
- Consider low dose steroids i.e. 10-20 pred during 1st 2 resumption cycles
Nephrotoxicity from Chemotherapy | BCNephro
Summary
Interstitial nephritis is a relatively common cause of Acute Kidney Injury. Medications are the common cause. Diagnosis requires clinical acumen as characteristic described findings are often absent. Renal biopsy may be needed to confirm diagnosis. In addition to stopping the culprit medication, treatment with steroids may be required. Immune checkpoint inhibitors can often be safely resumed after treatment. In these cases other medications associated with AIN such as proton pump inhibitors should be held.



