Table of Contents
I’m often referred patients with difficult to control hypertension and here’s my approach, things I think about when assessing these patients.
- I’m always considering a 24 hour ambulatory blood pressure monitor to exclude white coat effect.
- I need to make sure to do a careful medication review including over the counter medications. This is to assess for medications that can cause or aggravate hypertension and to make sure the patient is on an optimal antihypertensive regimen.
These first two things fall under the category of apparent resistant or pseudo resistant hypertension.
Is it White Coat Syndrome? Pseudo-resistant Hypertension @BCNephro
Pseudoresistant Hypertension | BCNephro
The next two things serve not only as an initial screen for secondary causes of hypertension, but also can help guide treatment. These are:
- A renal evaluation which should at minimum include a basic metabolic panel, urinalysis and imaging, most often a renal ultrasound
- A hormonal evaluation which usually includes an aldosterone and plasma renin activity, and in select cases may also include plasma free metanephrines.
I’m going to go into each of these in more detail and conclude with my stepped approach to treatment and tricks I have up my sleeve for difficult cases.
24 hour ambulatory blood pressure monitor.
The reasons to do this are to exclude:
- White coat hypertension: Blood pressure that is elevated in the health care setting, but at target without medications outside the office
- White coat effect: Blood pressure that is above target in the health care setting, but controlled to target with medications outside of the office.
It also assesses for nocturnal dipping. The blood pressure normally drops by at least 15% when we sleep, if it doesn’t drop by at least 10% the patient is classified as a “non-dipper”. Non dipping puts the patient at higher risk of adverse cardiovascular outcomes and also may be a clue of underlying obstructive sleep apnea.
Remember the normal 24 hour average is lower than that for an office or home reading, less than 125/75 as opposed to 130/80. This is to take into account the nocturnal dipping, the normal blood pressure decrease with sleep. These reports often breakdown:
- 24 hour average: Normal < 125/75
- Awake average: Normal < 130/80
- Sleep average: Normal < 110/65
Medication Review
Here, I’m looking for medications that can cause hypertension, such as:
- NSAIDS
- Angiogenesis/ VEGF inhibitors
- Tyrosine kinase inhibitors
- Estrogen containing contraceptives
- Decongestants
- Stimulants such as ADHD medications
I’m also looking for a suboptimal medication regimen which can occur if the patient is:
- Not on a diuretic
- On suboptimal medication doses, less than 50% of the maximum dose
- On medications that are not synergistic.
RAAS blockers, ACE- inhibitors or angiotensin receptor blockers, are synergistic with thiazide diuretics and calcium channel blockers, but not synergistic with beta blockers. Two RAS inhibitors, such as an ACE-I and ARB would not be synergistic.
Renal Evaluation
Kidney disease is the most common secondary cause of hypertension. My evaluation in resistant cases includes at a minimum a:
- Basic metabolic panel
- Urinalysis
- Renal imaging (most often an ultrasound)
The metabolic panel will reveal if there is abnormal kidney function and also allows us to assess for hypokalemia and metabolic alkalosis, which if present indicate the possibility of primary hyperaldosteronism.
There can be kidney disease without a decrease in GFR and a urinalysis and imaging assess for these.
An abnormal urinalysis may indicate an underlying glomerulonephritis and if significant proteinuria is present an RAS blocker should be included in the medication regimen unless contraindicated.
Renal imaging, typically a renal ultrasound, is an important part of my evaluation. This can show:
- Occult kidney disease, such as polycystic kidney disease, chronic hydronephrosis or sequelae of vesicoureteral reflux.
- Significant renal asymmetry, unilateral atrophy, can be a clue for underlying renal artery stenosis.
I typically don’t screen for renal artery stenosis with a doppler ultrasound, although I might consider it in the right clinical context. I don’t find this test to have a great sensitivity. If I have a high suspicion of renal artery stenosis, such as the presence of significant vascular disease (with or without an abdominal bruit), asymmetric kidney sizes with unilateral atrophy or high renin hypertension, a CT or MR angiography would be the preferred test.
Hormonal Evaluation
I find measuring the aldosterone and plasma renin activity (PRA) helpful.
The Aldosterone Renin Ratio is the screen for primary hyperaldosteronism. Remember this requires both:
- An elevated ratio, greater than 20-30 and
- A high aldosterone > 10
Be careful about finding a high ratio without an elevated aldosterone. This typically occurs when the plasma renin activity is very low, less than 0.5, which will drive the ratio.
How to Diagnose Primary Hyperaldosteronism @BCNephro
Primary Hyperaldosteronism | BCNephro
Even if the screen is negative, these tests can provide useful information.
- Low renin hypertension, PRA, less than 0.5-1.0, suggests the presence of salt sensitive hypertension and the need to add or intensify the diuretic regimen.
- High renin hypertension, a PRA > 5.8 can be an additional clue to the presence of renal artery stenosis.
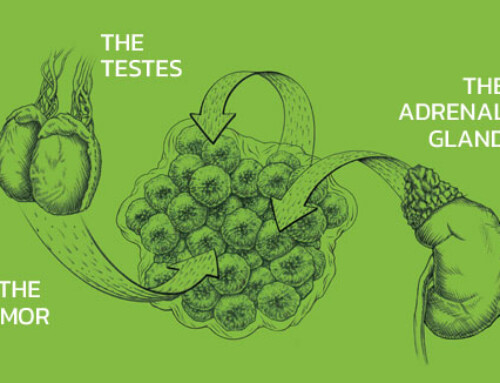
The other hormonal test is plasma free metanephrines. Pheochromocytoma is rare, but clues to its presence are paroxysmal hypertension with associated diaphoresis and tachycardia. These patients often also have orthostatic hypertension.
If you do this test remember there are a lot of false positives. When pheochromocytoma is present the elevation is typically very high > 4 times the upper limit of normal. Medications, such as tricyclics or physiologic stress can cause lesser elevations.
Stepped approach
An optimal stepped approach to antihypertensive medications is:
- RAS blocker (ACE inhibitor or Angiotensin Receptor Blocker) or thiazide (chlorthalidone, hydrochlorothiazide)
- Agent not used in step 1
- Dihydropyridine calcium channel blocker (amlodipine, extended release nifedipine)
- Mineralocorticoid Antagonist. I typically use spironolactone 25 mg dose, it’s more potent than eplerenone and most patients don’t get gynecomastia at this 25 mg dose. Remember to monitor closely for hyperkalemia, especially if the patient is also on an RAS blocker or not on a thiazide. I advise my patients to hold spironolactone if they are taking or need other medications that can raise potassium like NSAIDS or trimethoprim sulfa.
- Vasodilating beta blocker (carvedilol or nebivolol). I find metoprolol, although good for cardioprotection, is not a great antihypertensive and labetalol tends to have more adverse side effects.
- After this there are a couple of options.
- Use a long acting loop diuretic like torsemide if there still is a salt sensitive/ volume component. Need to use caution if combining with a thiazide which may lead to hypokalemia or an elevated creatinine. In most cases I don’t combine these two classes.
- Vasodilators such as minoxidil or hydralazine
- Alpha blockers such as doxazosin or prazosin
- Clonidine which although potent is not ideal because of its side effects and risk of rebound.
Tricks up my Sleeve
As a nephrologist I have some tricks up my sleeve, modifications I can make to the antihypertensive regimen that are often effective. These include:
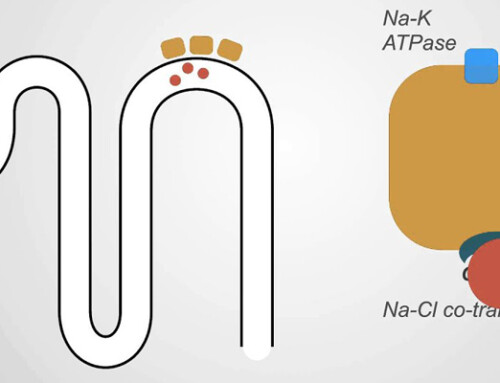
- Change Hydrochlorothiazide (HCTZ) to Chlorthalidone, at the same dose 25 mg per day. Chlorthalidone is more potent and has a longer halflife than HCTZ.
Is Chlorthalidone better than Hydrochlorothiazide? @BCNephro
Thiazide Diuretics, Chlorthalidone vs Hydrochlorothiazide | BCNephro
- If already on a loop diuretic such as furosemide options include
- Changing it to chlorthalidone, if the furosemide is low dose and there is no edema/ heart failure or
- Switching furosemide to the longer acting torsemide, if there is edema/ heart failure.
- Add spironolactone as the 4th agent. This is often effective in resistant hypertension even if there is not an elevated aldosterone renin ratio.
- Change a non dihydropyridine calcium channel blocker like diltiazem or verapamil to a nondihydropyridine like amlodipine or extended release nifedipine. Be mindful that if the nondihydropyridine is for tachycardia should make sure on a beta blocker. Anecdotally, I find nifedipine more potent than amlodipine and often change amlodipine to nifedipine.
- If on a beta blocker like metoprolol change to vasodilating beta blocker like carvedilol or nebivolol, unless there is a compelling cardiac indication for the former or a contraindication to the latter.
Summary
A nephrologist’s approach to hypertension. Exclude pseudoresistance with an ambulatory blood pressure monitor and medication review. Screen for secondary causes and guide treatment with a renal assessment and aldosterone renin ratio. Effective interventions include intensifying the diuretic regimen with chlorthalidone or torsemide, adding spironolactone and using a dihydropyridine calcium channel blocker and/or vasodilating beta blocker.