Table of Contents
Is protein bad for the kidney? Should protein be restricted? Are there downsides to restricting protein?
These questions will be addressed below.
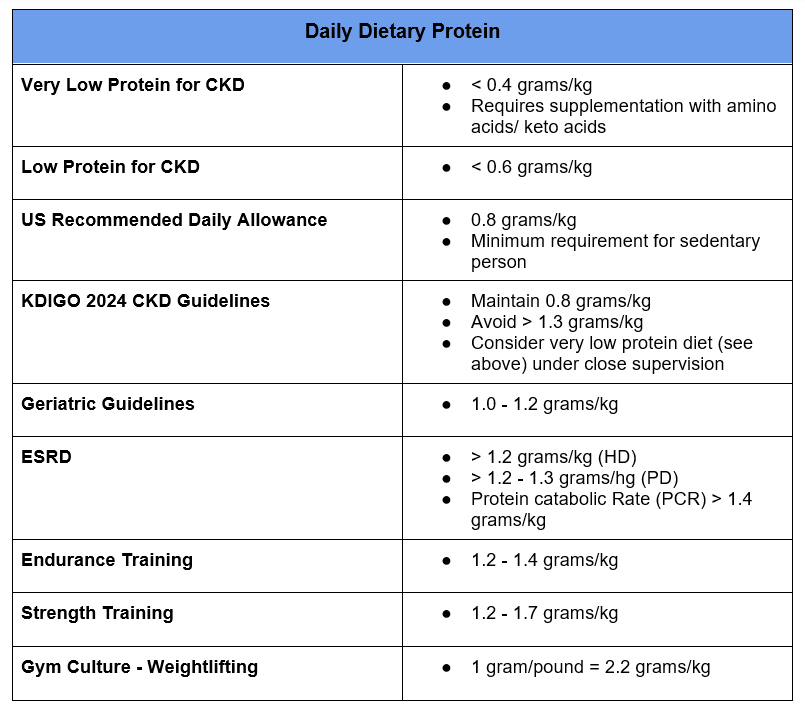
There are a wide range of recommendations for dietary protein intake for patients with Chronic Kidney Disease (CKD) and in general.
Reasons Why High Protein May be Harmful in Kidney Disease
There are several reasons why a high protein diet may be detrimental in kidney disease
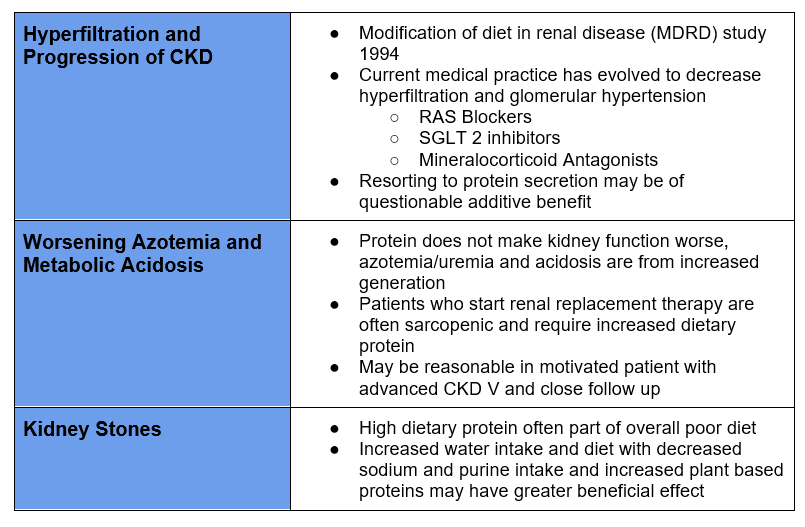
- Hyperfiltration leading to progression of Chronic Kidney Disease (CKD).
- Increased glomerular filtration (hyperfiltration) is maladaptive, potentially leading to proteinuria and glomerulosclerosis. Hyperfiltration is considered to be the initial pathophysiology leading to diabetic kidney disease. Diabetic Nephropathy | BCNephro
- Renin angiotensin system (RAS) blockers and SGLT2 inhibitors are reno protective because they reduce glomerular pressure and hyperfiltration by impairing constriction of the efferent arteriole (RAS blockers) and dilatation of the afferent arteriole (SGLT2 inhibitors) respectively.
- Protein (amino acids) cause dilatation of the afferent arteriole.
2. Worsening azotemia/uremia and acidosis.
Azotemia vs Uremia @BCNephro – YouTube
- Protein, particularly animal protein, is metabolized to urea, blood urea nitrogen (BUN) and increases acid production.
- This urea and acid needs to be excreted by the kidneys. In advanced CKD, the kidneys may not be able to excrete the excess urea and acid load.
Use of Renin Angiotensin System Blockers in CKD
3. Kidney stones.
- Animal protein metabolites can contribute to hypercalciuria increasing risk for calcium oxalate stones
- Animal protein metabolites result in increased renal acid excretion, contributing to hypocitraturia (increasing risk for calcium oxalate stones) and low/acidic urine pH (increasing risk for uric acid stones).
Perspective
Potential Downside of Protein Restriction
- Age related malnutrition and sarcopenia. We lose muscle mass as we age. Low muscle mass is associated with frailty and an increased mortality. Dietary protein needs to be coupled with resistance exercise to maintain/mitigate muscle loss.
- Difficulty achieving protein goals in patients with ESRD on renal replacement therapy. It is a challenge to maintain adequate dietary protein in patients on dialysis. It is also more difficult to regain as opposed to mitigate or slow losing muscle These goals may be more realistically achieved if patients had adequate dietary protein prior to initiating dialysis.
Summary
- I am convinced, and data supports that the quality of the food is more important than the precise amount of macronutrients specific components.
- Good sources of protein include lean meat (i.e. chicken), fish, low fat dairy, greek yogurt, eggs in addition to plant based proteins.
- I typically advise patients with CKD to maintain normal dietary protein (0.8-1.2 gram/kg/day). This is consistent with recent CKD guidelines.
KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease
- For advanced CKD stage 5 (pre dialysis) restricting dietary protein may be reasonable to mitigate azotemia/uremia and metabolic acidosis potentially forestalling the need for dialysis.
- For patients with recurrent kidney stones I advise avoiding excess dietary animal protein as a part of a general healthy diet with high water intake, sodium restriction, and plant based protein
- For patients who strength train (and myself) I advise 1.7 grams/kg/day as sufficient. Dietary protein in excess of this is often excreted and causes GI side effects.