Table of Contents
Can MRI contrast be safely given to a patient with kidney disease?
Iodinated contrast for CT or angiography is known to be associated with nephrotoxicity. Contrast Nephropathy does it exist? How to make it not happen | BCNephro
Therefore it is reasonable to have concerns regarding MRI contrast.
What is MRI Contrast?
MRI contrast is a substance called gadolinium. This differs from iodinated contrast.
- Gadolinium is a rare earth metal that has strong paramagnetic properties, making it ideal for MR imaging.
- Free gadolinium is toxic, therefore it must be chelated to an organic ligand to encapsulate the ion and reduce toxicity.
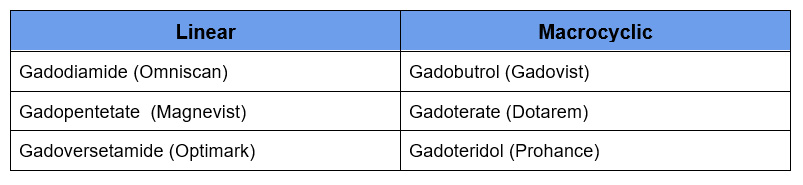
- These organic ligands can be either linear or macrocyclic, ionic or nonionic.
Gadolinium is normally eliminated by the kidneys with a half life of about 1 ½ hours.
Both linear and macrocyclic agents can be ionic or nonionic. This has to do with whether there is a covalent bond (nonionic) or not (ionic). Ionic agents tend to have a higher osmolarity. However, unlike iodinated contrast for CT or angiography this does not increase toxicity.
Both ionic and nonionic agents are hypertonic compared to plasma.
Is Gadolinium Nephrotoxic?
Gadolinium has been shown to affect glomerular filtration rate (GFR), however these effects are typically minimal, transient and not clinically significant. Therefore, gadolinium is not considered to be nephrotoxic.
For this reason MR angiography (in lieu of CT angiography) with gadolinium became the imaging of choice for patients with CKD, ESRD or AKI.
So, what is the problem with gadolinium and kidney disease?
Nephrogenic Systemic Fibrosis
Nephrogenic Systemic Fibrosis (NSF) was observed in patients with advanced CKD or ESRD. It is a scleroderma like condition often resulting in debilitating and even fatal tissue and organ fibrosis. It manifests as:
- Cutaneous thickening or indurated, discolored skin with plaques, papules and/or nodules.
- Affects trunk and limbs, in a bilateral, symmetric manner. Starts distal and progresses proximal. Spares face.
- Sclerodactyly and joint contractures may occur.
- Multiorgan involvement with internal organ fibrosis may occur.
Diagnosis can be confirmed by tissue biopsy which has characteristic findings.
The hypothesis is that the clearance of gadolinium is prolonged with a decreased GFR. With time and a prolonged half life free gadolinium is released and deposits in tissues resulting in toxicity.
It was observed that nephrogenic systemic fibrosis (NSF) was associated with linear, but not macrocyclic gadolinium agents. Macrocyclic ligands are more stable than linear ones, therefore associated with a lower risk of free gadolinium deposition. However, macrocyclic agents have a higher incidence of allergic reactions.
The different gadolinium agents were then classified by the American College of Radiology based on their risk of developing NSF.
- Group I – Greatest number of associated NSF cases
- Group II – Few, if any associated NSF cases
- Group III – Few, if any associated NSF cases, but limited data
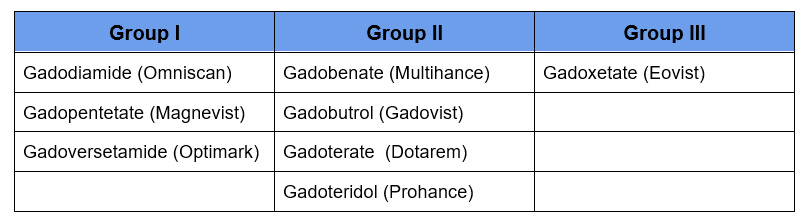
Group I agents are linear, Group II macrocyclic, with the exception of Gadobenate. The Group III agent Gadoxetate is typically used to evaluate liver lesions.
Regarding the risk of NSF the general consensus is:
- Any type of gadolinium is safe with an eGFR> 30
- Group II agents should be used with eGFR < 30 or ESRD
Gadolinium is cleared by dialysis, therefore some suggest scheduling dialysis in an ESRD patient after administration if possible. Most do not recommend extra dialysis or performing dialysis in a patient with AKI or CKD stage 4 or 5 not on dialysis.
The American College of Radiology 2023 statement regarding gadolinium begins on page 82 of the ACR Manual On Contrast Media
Some linear gadolinium agents interfere with the assay for calcium resulting in artificially low calcium values. This phenomenon may not be frequently observed as it is more likely to be found with prolonged gadolinium retention in patients with impaired renal function and linear agents are not used in these patients.
Gadolinium Deposition Disease
It has been noted that gadolinium can deposit in the brain in patients with normal kidney function. The clinical significance is not known. It appears to be more of an issue with repeated exposure, i.e. multiple MRI’s.
This can occur with both linear and macrocyclic gadolinium agents, although the extent of deposition may be higher with linear chelates.
Some have reported a clinical syndrome manifest by brain fog and paresthesias.
Summary
Gadolinium generally is not associated with nephrotoxicity. The concern is a condition called nephrogenic systemic fibrosis (NSF) believed to be a result of free gadolinium deposition with prolonged retention in patients with impaired renal function. There also is evidence of gadolinium deposition in the brain with repeated exposure in patients with normal renal function.
As with everything in medicine, the decision to perform an MRI with gadolinium should be carefully made considering potential risks and benefits. The risk of this condition with the newer macrocyclic, group II agents is low enough that the benefits of diagnosis outweigh the risk of NSF in many cases.



